Last Updated on: 2nd January 2026, 06:18 am
When a horizontal or vertical movement of a tooth is detected, it is referred to as tooth mobility. It is an oral health condition that is normal up to a certain point. If the movement exceeds that limit, it is interpreted as a symptom of a more complex condition in the gums and a loss of alveolar bone.
Dental mobility can have a physiological or pathological origin:
1. Physiological mobility: the natural movement a tooth presents, within a limit. It occurs most often in teeth that have only one root.
2. Pathological mobility: diagnosed when the loose tooth presents a movement that exceeds the limit considered normal.
What is the Limit of Tooth Mobility that is Considered Normal?
Dentistry uses a scale that allows for determining the degree of mobility of a tooth while diagnosing the treatment to follow. For this purpose, a four-level scale is used:
• Grade 0 – It is considered normal, physiological mobility.
• Grade 1 – Horizontal movement is recorded between 1 millimeter or less.
• Grade 2 – There is horizontal movement greater than 1 millimeter.
• Grade 3 – There is horizontal and vertical movement. The tooth moves in different directions.
Tooth mobility is a sign of advanced periodontal disease, also known as chronic periodontitis, a condition that affects the tissues that provide support and stability to the teeth, such as the periodontal ligament and alveolar bone.
In other words, dental mobility is a sign of significant, relevant loss of the tissues that support the teeth.
In most cases, dental mobility does not present pain; but if care is not given, it can lead to a critical oral health condition, with the loss of one or more teeth.
Why does Tooth Mobility Occur?
In the initial stage of gum disease, the dentist diagnoses gingivitis, a pathology that may be reversible with relevant dental treatment, such as dental prophylaxis together with the practice of adequate oral hygiene that facilitates the elimination of bacterial plaque and calculus.
• If gingivitis is not treated, the disease evolves into chronic periodontitis, a condition that increases over time and is not reversible.
• The teeth may separate from the gums such that pockets form in the space remaining. It can become infected, deepen, and finally affect the supporting tissues (gums and bone) such that the teeth loosen, promoting dental mobility.
• Gum disease is one of the main causes of tooth loss in the adult population. Chronic periodontitis is estimated to affect 47% of people over the age of 30 in the United States.

What are the Causes of Dental Mobility?
Dental mobility can be a consequence of various circumstances:
1. Accidents and injuries.
2. Dental absences that cause the inadequate position of the other teeth, facilitating abnormal contact.
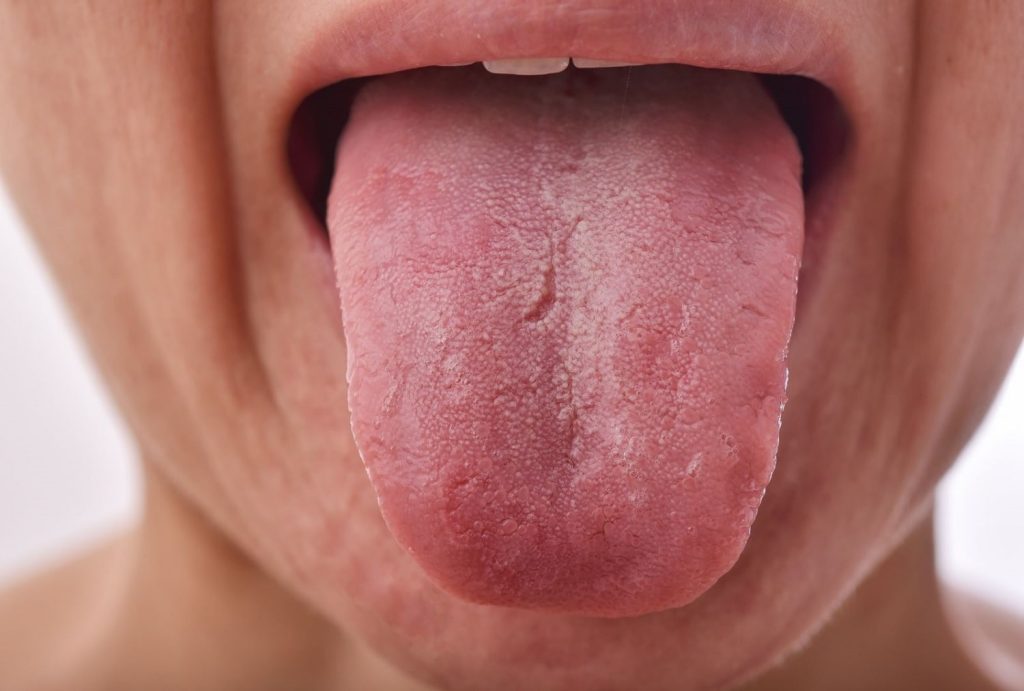
3. Bruxism and tongue pressure, parafunctional habits that affect the periodontal ligament.
4. Constant stressful situations.
5. Chronic periodontal disease and inflammation of the periodontal ligament.
6. Systemic diseases and their treatments, such as diabetes, cancer, and HIV.
7. Poor oral hygiene that facilitates the formation of dental plaque and calculus.
8. Traumatic occlusion (malocclusion). an inadequate alignment of the teeth hinders oral hygiene, facilitates premature wear, and promotes dental caries.
9. Osteoporosis affects the density of the bones and can affect the condition of the maxillary bone tissue.
10. Improper use of orthodontic appliances.
Different studies have established a relationship between tobacco use (smoking) and predisposition to periodontal disease, with its corresponding effect on dental mobility.
Symptoms of Tooth Mobility

Although the obvious sign of this condition is a loose tooth, other signs warn of an underlying health condition: chronic periodontitis:
1. Difficulty in chewing food.
2. Teeth with a longer appearance, due to receding gums.
3. Pain in the affected tooth.
4. Red gums around the affected tooth.
What are the Treatments for Dental Mobility?
The treatment depends upon the degree of dental mobility that occurs.
There are therapeutic alternatives – surgical and non-surgical – such as scaling and root planing, pocket reduction surgery, and soft tissue and bone grafts.
1. Surgery
Pocket reduction is the treatment option when the expected result has not been achieved with non-surgical procedures. This intervention makes it possible to reduce the depth of the pocket and save the teeth. It also facilitates the removal of tartar in the inner part of the gums. Sometimes this procedure is combined with regenerative therapies that stimulate the growth of tissue osseous.
2. Bone grafting
Grafts of soft tissue and bone can restore the support structures and protect the dental roots that may be exposed and generate more complex situations.
We have a comprehensive guide about dental bone graft procedures that can help you understand more about this treatment.
The complementary procedure to these therapeutic alternatives is to directly treat periodontal infections that cause dental mobility.
How can Tooth Mobility be Prevented?

Preventing tooth mobility reduces the chances of periodontal or gum disease. Some preventative tactics should be implemented:
• Brush your teeth at least tawice a day with fluoride toothpaste.
• Floss daily to remove plaque and food debris that can later form tartar and calculus.
• Avoid or reduce tobacco use.
• Renew dental fillings that show deterioration.
• Treat those teeth affected by cavities.
• Use mouthwash.
• Periodically visit the dentist to facilitate early diagnosis and timely treatment.
When Should you See a Dentist?
Dental mobility as an oral health condition can be the consequence of various circumstances, and it compromises dental support tissues (ligaments and maxillary bone), affecting the stability of the teeth.
Control and preventive treatment reduce the impact of the condition or injury that causes dental mobility and stop its progress.
If a tooth displays unusual movement, or the dental piece is loose, it is pertinent to consult with an oral health professional since it may be a case of pathological dental mobility.
It is important to pay attention to pathological dental mobility to prevent it from progressively progressing to a more complex clinical picture.
Conclusion
Tooth mobility is a common oral health problem that may be caused by a variety of factors, including periodontal disease and dental trauma. It is important to recognize the symptoms of tooth mobility and seek early treatment to prevent tooth loss and other complications.
In addition, prevention is key in the fight against dental mobility through good oral hygiene and control of risk factors, such as smoking and systemic diseases.
Frequently Asked Questions
Can tooth mobility be fixed?
The treatment depends upon the degree of dental mobility that occurs. There are therapeutic alternatives, surgical and non surgical, such as scaling and root planing, pocket reduction surgery, and soft tissue and bone grafts.
What causes a tooth to be mobile?
Tooth mobility can be caused by several circumstances: accidents and injuries, missing teeth causing improper positioning of other teeth, bruxism, tongue pressure, constant stress, chronic periodontal disease, systemic diseases such as diabetes, cancer and HIV, poor oral hygiene that favors the formation of plaque and calculus, traumatic occlusion (malocclusion), osteoporosis that affects bone density, and improper use of orthodontic appliances.
Can tooth mobility cause pain?
The obvious sign of this condition is a loose tooth, other signs warn of an underlying health condition: chronic periodontitis, Difficulty chewing food, Teeth with a longer appearance, due to receding gums, Pain in the affected tooth, Red gums around the affected tooth.
What is class 3 tooth mobility?
The class 3 mobility is horizontal and vertical movement. The tooth moves in different directions.
What is class I, II, and III mobility on teeth?
- Grade 1: Horizontal movement is recorded between 1 millimeter or less.
- Grade 2: There is horizontal movement greater than 1 millimeter.
- Grade 3: There is horizontal and vertical movement. The tooth moves in different directions.
Share:
References
1. Botero J E, Bedoya E. (August 2010). Determinants of periodontal diagnosis. Clinical journal of periodontics, implantology and oral rehabilitation.https://www.scielo.cl/scielo.php?script=sci_arttext&pid=S0719-01072010000200007
2. Boatman Leticia, Velez Maria Eugenia, Alvera Fanny Stella (June 2008). Prognostic factors in periodontium. Journal Faculty of Dentistry University of Antioch.
3. Coelho Renata, Santos Estela, Cimoes Renata et al. (December 1, 2011) Tooth mobility in chronic periodontitis. https://www.actaodontologica.com/ediciones/2011/4/art-11/
4. Mouthhealthy. (s.f). Gum Disease. https://www.mouthhealthy.org/all-topics-a-z/gum-disease/
5. T Fleszar, J Knowles, E Morrison, F Burgett, R Nissle, S Ramfjord (1980). Tooth mobility and periodontal therapy.
https://pubmed.ncbi.nlm.nih.gov/6938529/
6. Yazan Hassona, Mohammad Wael Saleh, Hamza Alkhawaldeh, Ruba Al Abweh (s.f.). Unusual cause of tooth mobility. https://casereports.bmj.com/content/13/12/e235086
- Nayibe Cubillos M. [Author]
Pharmaceutical Chemestry |Pharmaceutical Process Management | Pharmaceutical Care | Pharmaceutical Services Audit | Pharmaceutical Services Process Consulting | Content Project Manager | SEO Knowledge | Content Writer | Leadership | Scrum Master
View all posts
A healthcare writer with a solid background in pharmaceutical chemistry and a thorough understanding of Colombian regulatory processes and comprehensive sector management, she has significant experience coordinating and leading multidisciplina...Recent Posts