Last Updated on: 27th December 2025, 06:42 am
Antibiotics for tooth infection often require addressing the issue effectively. The most common reasons for dental visits are dental caries, dental abscesses, gingivitis, or periodontitis, which result from infectious oral conditions. Dental infection – also called odontogenic infection – is caused by bacterial invasion of the pulp space (the nerve); Generally, the culprits are advanced caries, an unsuccessful root canal treatment, or an advanced chronic infection (periodontitis), among others.
The infection may be concentrated in the nerve space or spread to surrounding tissues, frequently affecting the third molars, known as wisdom teeth.
People with a depressed immune system (diabetes, infectious endocarditis, lupus, cancer, HIV) and the elderly are at greater risk of spreading dental infection.
The World Health Organization (WHO) in its global report on the state of oral health (2022), points out that in the world oral diseases affect approximately 3,500 million people.
The WHO report states that worldwide 2,000 million people suffer from caries in permanent teeth and 514 million children have caries in primary teeth.
What are the Symptoms?
• Forever
• Fatigue
• General discomfort
• Swollen jaw or neck
• Severe pain that does not go away
These are some of the symptoms of advanced dental infection.
When to use antibiotics for tooth infection?
To make appropriate use of antibiotics and avoid bacterial resistance to their curative effects, the WHO recommends limiting their prescription to the necessary cases. On the other hand, the American Dental Association (ADA) recommends avoiding the use of antibiotics due to their possible side effects.
The prescription of antibiotics is a part of the healing process accompanied by other procedures. It must be taken into account that the infected tooth does not always require antibiotics. In some cases, a dental infection can be treated with drains, deep cleanings, or a root canal (the removal of infected tissue).
The treating dentist has the alternative of prescribing antibiotics in the following cases:
• To perform a procedure to prevent the risk of the infection spreading to other areas. It is a frequent measure for people who have a depressed immune system.
• In the treatment of dental infections when other treatments for acute infections – such as ulcerative gingivitis or periodontitis – do not achieve the expected response.
If the dental infection spreads or a clinical picture with a low level of defense is indicated, the dentist can prescribe antibiotics, to prevent further effects and health complications.
What Happens if Left Untreated?
If a dental infection is not treated promptly, it can lead to other more complex health conditions, such as:
• Soss of teeth
• Blood infection
• Pneumonia
• Brain infection
• Endocarditis
What are the Antibiotics for Tooth Infections?
Currently, multiple strains of the bacteria are known to grow in the mouth. This determines the type of antibiotic formulated to combat the microorganism that causes the infection.
For this process, the health status and age of the patient must be taken into account. Special care is necessary for pregnant women, children, and people with renal failure, all conditions that determine the choice of the indicated antibiotic treatment.
Here are some of the antibiotics used to treat dental infections:
1. Oral amoxicillin / Oral potassium penicillin V
The ADA recommends them as first-line drugs. It belongs to the group of penicillin-like drugs that fight infections by preventing the spread of bacteria. However, this type of medication is not indicated for treating viral infections.
In cases of bacterial resistance to amoxicillin, this drug is combined with clavulanic acid to increase its effect. The acid prevents the bacteria from destroying the antibiotic medicine. This combination can reduce the effectiveness of oral contraceptives, which is why during treatment, it is recommended to resort to other mechanisms.
2. Amoxicillin
It is contraindicated for people allergic to penicillin. In these cases, the health professional must choose a substitute drug, such as:
3. Azithromycin
It is a mediation with good results in the treatment of a variety of dental tissue infections since it stops the growth of bacteria. It should not be prescribed with clindamycin, as the effect is canceled. It should be noted that this drug is contraindicated in people with liver conditions.
4. Cephalexin
This antibiotic inhibits the enzymes of the bacterial cell wall and interrupts their synthesis. It is a useful medication for the treatment of dental infections but should not be prescribed to people with kidney failure, liver disease, or pregnant women.
5. Clindamycin
It is an effective medicine against different infectious bacteria. A study conducted in 2015 points out that some researchers recommend it for the treatment of dental infections due to low bacterial resistance.
6. Erythromycin
It is a medication of wide formulation. It is frequently prescribed for the treatment of cavities and plaque bacteria. In some cases, it is used for the treatment of dental abscesses. People taking terfenadine, astemizole, or cisapride should not receive erythromycin.
7. Metronidazole
This medication is frequently prescribed to treat a variety of dental infections, although some professionals note that it is not a first-line option for treatment. Caution should be used when prescribed with alcohol, anticoagulants, seizure control drugs, sedatives, and medications for depression.
For people with liver or intestinal diseases, disorders of blood cells, or the nervous system, it is necessary to consider other antibiotic drugs.
Side Effects of Antibiotics for Tooth Infection
Some of the side effects that treatment with antibiotic drugs can generate are:
• Advancement of dental infection
• Change in taste
• Diarrhea
• Difficulty breathing
• Headache
• Joint pain
• Rash
• Swelling of the face, eyes, or mouth
• Yeast Infection/candidiasis
• Nausea
• Wheezing
• Urticaria
If any of these symptoms occur, consult your health professional to follow the relevant protocol and avoid other health conditions.
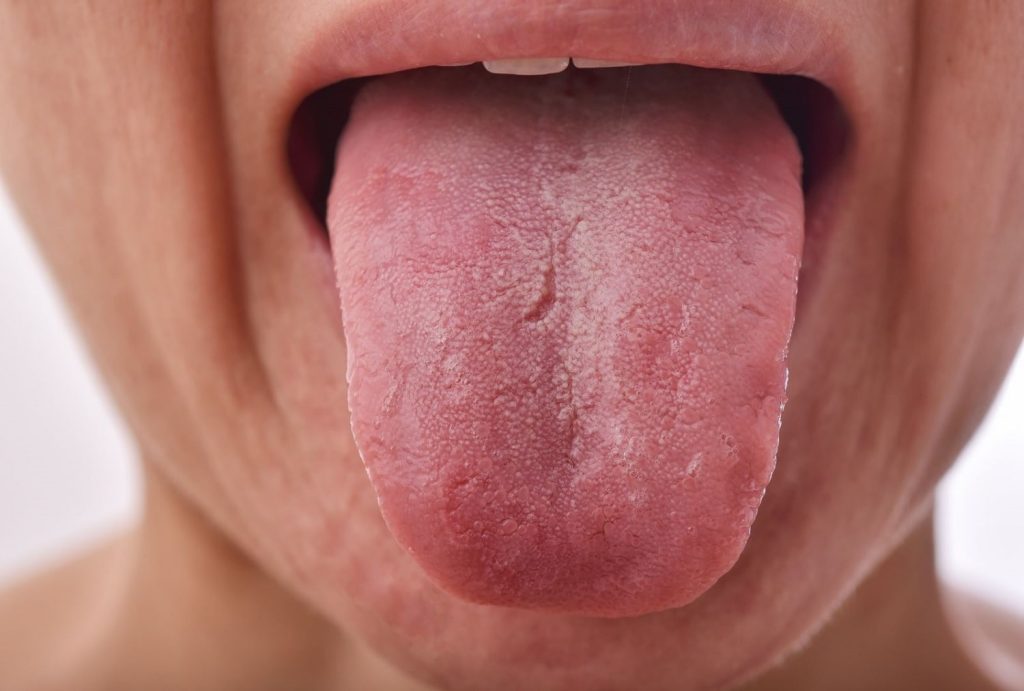
Prevention of Dental Infections
• The best way to prevent a dental infection is to practice good oral hygiene. It is recommended to brush your teeth twice a day with toothpaste containing fluoride.
• Use dental floss or interdental brushes to remove bacterial plaque.
• Limit sugar intake, especially between meals.
• Doctors should be mindful of prescribing sugary medications to avoid the risk of dental caries.
• For people with a dry mouth, low-sugar artificial saliva or sugar-free gum may be indicated.
• Replace the sugar with other sweeteners, such as birch sugar (xylitol).
• Regularly visit the dentist for cleaning sessions and preventive reviews.
Any of the aforementioned antibiotics for tooth infection should be evaluated and prescribed by your dentist for safety. It is important to ask the dentist’s pharmacist how it should be administered and the most common side effects to be aware of. Also, consult with these professionals on how to manage pain if present since antibiotics fight bacteria, but they do not work for pain management.
Frequently Asked Questions
Common antibiotics used for dental abscesses include:
- Amoxicillin: This first-line antibiotic is often combined with clavulanic acid to broaden its spectrum of action against oral bacteria.
- Azithromycin: Another first-line option, particularly useful for patients allergic to penicillin.
- Cefoxitin: A cephalosporin antibiotic effective against a wide range of oral bacteria.
- Clindamycin: Used as an alternative in case of penicillin allergy or when other antibiotics are ineffective.
- Metronidazole: Particularly effective against anaerobic bacteria, common in oral infections.
- Penicillin: A classic antibiotic still used in some cases of dental abscesses.
It is crucial to note that:
The specific antibiotic chosen depends on the individual patient and the characteristics of the abscess.
Self-medicating with antibiotics is strongly discouraged, as it can lead to antibiotic resistance and other serious consequences.
Only a qualified healthcare professional can properly diagnose and treat a dental abscess.
What is the Strongest Antibiotic for a Tooth Infection?
Amoxicillin is typically the first choice for treating a tooth infection. For more severe infections, your dentist might prescribe a combination of amoxicillin and clavulanate, known as Augmentin. This combination is more potent and provides enhanced effectiveness against tooth infections.
What is Triple Antibiotic for Tooth Infection?
Triple antibiotic paste (TAP), which includes metronidazole, ciprofloxacin, and minocycline, has been shown to be effective in controlling root canal pathogens and managing non-vital young permanent teeth. This combination is a successful regimen for treating severe tooth infections.
What is the Best Antibiotic for Dental Work?
When it comes to dental work, your dentist will select an antibiotic that effectively eliminates your infection. Penicillin-class antibiotics, such as penicillin and amoxicillin, are the most commonly used to treat tooth infections. Additionally, metronidazole may be prescribed for specific types of bacterial infections.
Share:
References
1. Cadman, Bethany (Junio 2 de 2018) How do you know if you have a cracked tooth? / https://www.medicalnewstoday.com/articles/321259
2. Chao, Sally (Enero 23 de 2023) What are the best antibiotics for a tooth infection? / https://www.drugs.com/medical-answers/best-antibiotics-tooth-infection-3555997/
3. Dorwart, Laura (Marzo 23 de 2022) Antibiotics for Tooth Infection: What You Should Know / https://www.verywellhealth.com/antibiotics-for-tooth-infection-5220697
4. MedlinePlus (Agosto 15 de 2018) Amoxicillin and Clavulanic Acid / https://medlineplus.gov/druginfo/meds/a685024.html
5. Robles, Purificación / Echaniza Elena et al (April 2013) I’m going to the dentist: antibiotic as prevention or as treatment? Primary Care Magazine, Volume 45 – No. 4 / https://www.sciencedirect.com/science/article/pii/S0212656712004155#section-cited-by
6. Robertson, Douglas/Keys, William et al (March 2015). Severe Acute Dental Infections / https://www.intramed.net/contenidover.asp?contenidoid=86577&pagina=1
7. Rodríguez-Alonso, Elías (2009) Antibiotic treatment of odontogenic infection / https://www.sanidad.gob.es/biblioPublic/publicaciones/recursos_propios/infMedic/docs/vol33_3TratAntibInfecOdont.pdf
8. Technologies for health (June 21, 2018) Specific antibiotics for dental infections and contraindications / https://tecnologiaparalasalud.com/antibioticos-especificos-infecciones-dentales/
- Nayibe Cubillos M. [Author]
Pharmaceutical Chemestry |Pharmaceutical Process Management | Pharmaceutical Care | Pharmaceutical Services Audit | Pharmaceutical Services Process Consulting | Content Project Manager | SEO Knowledge | Content Writer | Leadership | Scrum Master
View all posts
A healthcare writer with a solid background in pharmaceutical chemistry and a thorough understanding of Colombian regulatory processes and comprehensive sector management, she has significant experience coordinating and leading multidisciplina...