Last Updated on: 27th December 2025, 07:48 am
Some people consult the dentist concerned about the health of their gums. This includes the signs and symptoms of gum disease. Gingival inflammation and bleeding are frequent conditions, but is it normal for gums to become inflamed and bleed? The answer is NO, and below we explain why:
What are Gum Diseases?
Teeth are anchored to the maxillary bones, and these in turn are covered by gum tissue. Gums are a soft, pink tissue that lines the bone that supports the teeth. Gum diseases can affect these tooth-supporting tissues, and in very advanced stages, can cause tooth loss.
What Causes Gum Diseases?
Bacterial plaque is a film or layer of bacteria and food that adheres to the teeth, especially near and under the gums. When it is not properly removed with brushing or flossing, it hardens and forms what is known as calculus or tartar. This calcified or hardened plaque can only be removed in the dental office with specialized instruments and equipment.
It is necessary to visit the dentist every 6 months to keep the teeth free of these factors that can cause gum disease.
The presence of this soft or hard bacterial plaque causes the gums to become inflamed and diseased, leading to other oral health problems. Although this is the main factor in developing gum diseases, it is not the only one. The following are other factors that can cause gum diseases:
1. Poor oral hygiene
When not all dental plaque is removed with brushing and flossing, the gums become inflamed.
2. Hormonal changes
Occur during pregnancy, puberty, menopause, and menstruation. These make the gums more sensitive, which facilitates the development of gum diseases.
3. Immune system disorders
Some pathologies compromise or affect the immune system such as HIV, lupus, cancer, arthritis, and/or diabetes, among others. This causes the body to not be able to respond adequately to an infection and both the gum and bone deteriorate more quickly.
4. Medications
Many studies have been carried out describing how medications can affect oral health, as some decrease the flow of saliva, which under normal conditions has a protective effect on the teeth and gums. Others can cause abnormal growth of gum tissue, such as phenytoin.
5. Smoking
Cigarettes contain nicotine, which negatively affects blood circulation in the gums, making the tissues less responsive to infections.
6. Family history
Some patients have a genetic predisposition to suffer from gum diseases. This does not mean that all patients with family history will suffer from gingival disease, but they are more susceptible to it.
7. Age
Older adults may have a higher risk of oral health problems, especially when physical and/or mental deterioration is present, which makes oral hygiene more difficult.
8. Bruxism
Grinding teeth can overload the supporting tissues and cause gum disease.
9. Tooth loss
The presence of gaps without teeth in the mouth makes it easier for food to accumulate in this area, causing damage to the gum and bone that support the adjacent teeth. Additionally, when some teeth are lost, those that remain must support all the forces of chewing, and this can weaken the tissues that support the teeth.
What Bacteria Cause Gum Disease?
In a healthy mouth, there is usually a significant population of bacteria, which is called the oral microbiota. Its function is to keep the mucous membranes healthy, aid in food metabolism, and promote the immune system, among other essential functions for overall health.
However, when there is poor oral hygiene, some bacteria grow uncontrollably and can induce inflammation and gum disease. Some of these bacteria are Porphyromonas gingivalis, Treponema denticola, Tannerella forsythia, and Aggregatibacter actinomycetemcomitans.
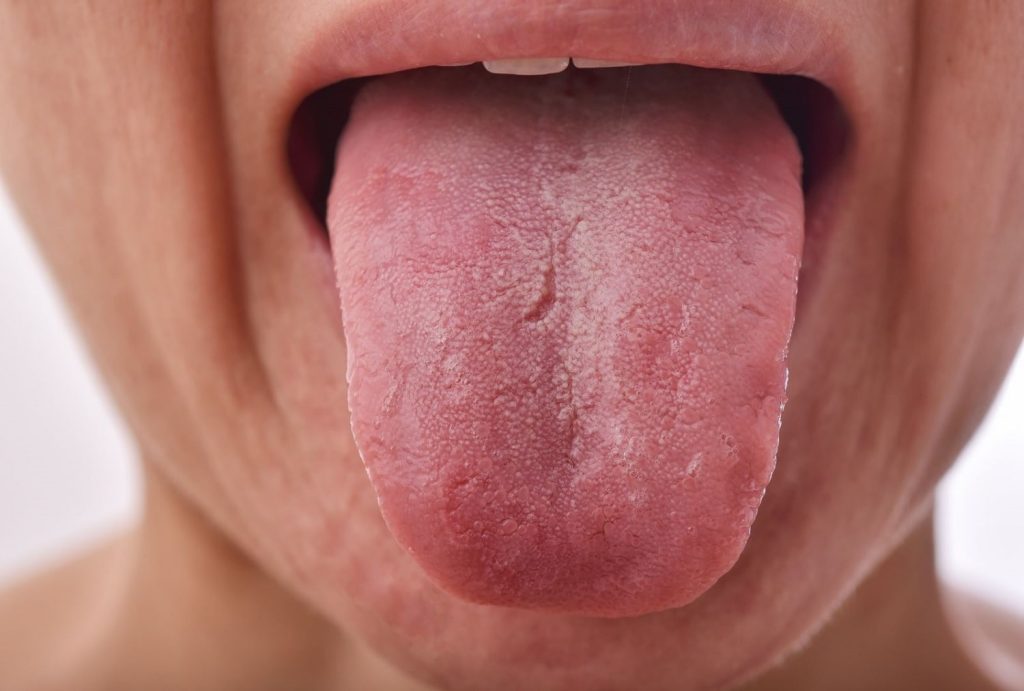
What are the Signs and Symptoms of Gum Disease?
The main signs of gum disease are as follows:
1. Red gums: Healthy gums have a light pink color, while inflamed gums appear reddish.
2. Swollen gums: Increased size of the gums.
3. Gingival bleeding: Gums that bleed easily when touched, when using dental floss, or when brushing teeth.
4. Sensitive gums: Pain when touching the gums or during brushing.
5. Bad breath: The presence of communities of bacteria living in the mouth releases some toxins that generate an unpleasant odor.
6. Receding gums: Smaller gums or longer teeth may be observed. This happens when gum disease has advanced so much that the roots of the teeth are partially exposed.
7. Sensitive teeth: Sensitivity or dental pain when consuming cold or hot foods because the gums recede and part of the roots of the teeth is exposed.
8. Loose teeth: When gum inflammation is not resolved, they decrease in height along with the underlying bone, so the support of the teeth is affected, and they begin to loosen.
What are the Types of Gum Disease?
According to the progression of the disease, two types of gum disease can be distinguished:
1. Gingivitis
It is the generalized or localized inflammation of the gums. In this, the level of the gum is still adequate, and there is no mobility of the teeth yet. During gingivitis, the signs and symptoms of early gum disease appear as gingival inflammation and mild bleeding.
2. Periodontitis
When gingivitis is not treated, this infection is deposited under the gums and reaches the bone. This causes the tissue that holds the tooth to be damaged, and the teeth begin to move. If the gum damage is severe, and a considerable amount of bone is lost, the teeth may fall out.
Who is at Higher Risk of Developing Gum Disease?
Some people with certain diseases or habits may be more likely to develop gum disease, such as:
• Smokers
• People with high stress levels.
• Patients diagnosed with diabetes, arthritis, heart disease, and immune system disorders such as HIV infections.
• People who do not have good dental health habits.
• People with crooked teeth, loose implants, or permanent dental appliances such as bridges that do not fit well.
• Family history of gum disease or early tooth loss.
• People who do not regularly visit the dentist (it is recommended to visit every 6 months).
• People with dental crowding or spacing (crooked or spaced teeth).
Who Treats Gum Disease?
Gum disease and supporting tissue conditions are treated by dentists who specialize in periodontics. They focus on removing bacterial plaque and calculus, restoring gum and periodontal health.
What is the Treatment For Gum Disease?
The solution for gum disease is good oral hygiene. After proper dental cleaning, if good hygiene habits are maintained, the gums will gradually disappear and stop bleeding. However, when gum disease progresses to the point of destroying the bone that supports the tooth, it is not possible to recover the lost tissue. Nevertheless, with deep cleaning, regular maintenance, and good management of dental hygiene at home, gum disease can be stopped and tooth loss avoided. In severe cases, the specialist may consider the use of gum or bone grafts to recover tooth support and improve aesthetics.
What Happens if Gum Disease is Left Untreated?
When gingivitis, which is the first stage of inflammation, is left untreated, the disease progresses to periodontitis. When plaque stays for a long time in the space between teeth and gums, painful infections can occur, generally leading to tooth loss. Other times, teeth loosen until they are lost, without any pain. To learn more about the stages of gum disease, click here.
How to Prevent Gum Disease?
Some strategies to prevent gum disease are:
1. Maintaining strict oral hygiene: The only way to remove dental plaque is through mechanical removal. This means that to ensure gum health, teeth must be brushed three times a day, making sure that the bristles of the brush clean all surfaces. Similarly, proper use of dental floss will help remove food debris and bacteria that are between teeth.
2. Use of alcohol-free mouthwashes: These can help disinfect the mouth and improve breath.
3. Replacing missing teeth: Whenever there is tooth loss, it is important to replace it, to balance the chewing forces and prevent plaque buildup in those spaces.
4. Brushing teeth vertically: Sometimes, when teeth are brushed horizontally (from front to back), gum recession can occur. Therefore, it is recommended to brush the bottom teeth up and the top teeth down.
5. Correcting bad dental positions: The use of orthodontics (braces) to straighten teeth that are twisted and too close or too far apart will cause less food to accumulate between teeth and make hygiene easier, promoting gum health.
6. Avoiding teeth grinding (bruxism): Seeking strategies for stress management and attending dental consultation to receive advice on this condition.
Conclusion
Among gum diseases, gingivitis is the most common, reversible, and less harmful form, but if not properly treated, it can progress to a more severe disease called periodontitis. This latter is an irreversible stage that leads to more severe damage such as tooth loss. Therefore, it is essential to maintain good oral hygiene and attend dental consultations every 6 months, so the dentist can remove hard and soft plaque that accumulates in hard-to-reach areas.
Frequently Asked Questions
What is gum disease and what are its main signs?
Gum disease, known as gingivitis in its early stages and periodontitis when it is more advanced, affects the tissues that surround and support the teeth. The main signs include red and swollen gums, easy bleeding, persistent bad breath, gingival retraction, and in advanced stages, tooth movement.
What are the common causes of gum disease?
The main causes include plaque and tartar buildup due to poor oral hygiene, hormonal changes, immune system disorders, the use of certain medications, smoking, and genetic predisposition. These factors contribute to inflammation and eventual degradation of gingival and bone tissue.
How is gum disease treated?
Treatment for gum disease varies depending on its severity. Initial measures include a professional cleaning to remove plaque and tartar, followed by a strict oral hygiene routine. In more severe cases, more intensive procedures such as scaling and root planing may be required, and in extreme situations, periodontal surgery to regenerate lost tissue.
What complications can arise if gum disease is not treated?
If left untreated, gingivitis can progress to periodontitis, which can lead to the destruction of bone and tooth-supporting tissue. This can cause tooth mobility, tooth loss, and may increase the risk of systemic complications such as heart disease and diabetes due to chronic inflammation.
How can I prevent gum disease?
Prevention is key and is achieved by maintaining meticulous oral hygiene that includes regular brushing, flossing, and mouthwashes. It is essential to visit the dentist regularly for professional cleanings and checkups. In addition, avoiding tobacco and properly managing health conditions that affect the immune system contribute to maintaining gum health.
Share:
References
1. Gingivitis. (Reviewed Ene 23, 2023). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/10950-gingivitis-and-periodontal-disease-gum-disease
2. Gum Disease Risk Factors. (Feb 7, 2020). American Academy of Periodontology.https://www.perio.org/for-patients/gum-disease-information/gum-disease-risk-factors/
3. Gum Disease Prevention. (Feb 8, 2020). American Academy of Periodontology.https://www.perio.org/for-patients/gum-disease-information/gum-disease-prevention/
4. Gum Disease and Other Diseases. (Jun 21, 2019). American Academy of Periodontology. https://www.perio.org/for-patients/gum-disease-information/gum-disease-and-other-diseases/
5. Non-Surgical Treatments. (Jun 21, 2019). American Academy of Periodontology.https://www.perio.org/for-patients/periodontal-treatments-and-procedures/non-surgical-treatments/
6. Periodontal Diseases. (s. f.). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/periodontal-diseases
7. Troncoso, C. M., Castillo-Ruiz, M., Daille, L. K., Fuentevilla, I. A., & Bittner, M. (2010). Co-detección de patógenos periodontales en pacientes chilenos con periodontitis crónica. Revista clínica de periodoncia, implantología y rehabilitación oral, 3(3), 118-122.
- Nayibe Cubillos M. [Author]
Pharmaceutical Chemestry |Pharmaceutical Process Management | Pharmaceutical Care | Pharmaceutical Services Audit | Pharmaceutical Services Process Consulting | Content Project Manager | SEO Knowledge | Content Writer | Leadership | Scrum Master
View all posts
A healthcare writer with a solid background in pharmaceutical chemistry and a thorough understanding of Colombian regulatory processes and comprehensive sector management, she has significant experience coordinating and leading multidisciplina...