Last Updated on: 30th December 2025, 08:45 am
Management of tooth dislocation is not far from everyday life, just like the dislocation or sprain of the shoulder, elbow, hand, foot, or hip. It can be a situation that occurs at any time and requires appropriate and timely treatment.
Tooth dislocation or tooth luxation occurs when the tissues, ligaments, or bones that support the tooth are injured, it can also affect the tooth’s nerves and blood supply. Falls and accidents can be the origin of dental dislocation. Below you will find a brief clinical description of the origin and the management of tooth dislocation.
What is a dental dislocation and what parts of the tooth can it affect? What are the consequences and treatment options? These are some of the questions that arise regarding these oral health incidents. Here you find the answers and information that guides you in handling the circumstance.
Falls, accidents during sports, or a trip can be the cause of a dislocated tooth.
Who are the most affected people?
This type of trauma occurs regularly in children, affecting the primary dentition, and can have effects on the permanent (secondary) dentition process. Cases are also reported in young adults, although this circumstance can occur at any time in life.
It is important to highlight that dental dislocation has a lower prevalence in women. In other words, it is more common in men. The identified causes give a clue about the origin of this difference in the incidence of cases.
Causes of tooth dislocation
According to the follow-up exercises that have been carried out in cases of dental luxation, the most frequent situations are:
• Assaults or violent attacks.
• Bicycle accidents.
• Traffic accidents (car, motorcycle)
• Accidents in the practice of rough sports
What parts of the tooth can be affected?
Dental dislocations have an impact on the soft tissues, the periodontal ligaments, the bone, and the pulp of the tooth.
Consequences of dental dislocation
The most commonly seen repercussions are:
• Destruction of the pulp canal
• Pulp necrosis
• Tooth loss
• Isolated, white, or opaque-looking spots and small pits (hypoplasia) may be present, revealing less tooth enamel.
• Enamel discoloration with a yellow-brown appearance.
The symptoms
These depend on the type of luxation that affects the tooth. The most common signs are:
• Loose tooth
• Loose tooth or with some change in its original location
• Discoloration of the dental piece.
• Pain or sensitivity in the tooth.
• Bleeding around the gums.
• High-pitched metallic sound when touching the tooth
If any of these conditions are evident, a dentist should be consulted to diagnose the required treatment.
The diagnosis
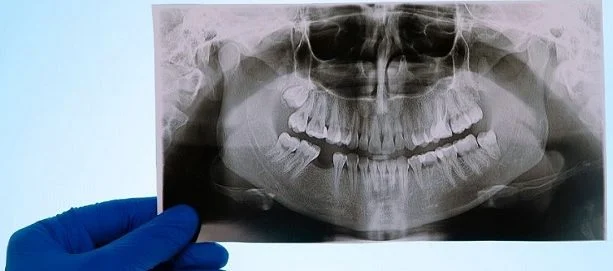
To reach the most accurate opinion, the oral health professional will ask about the symptoms or situation causing the dislocation. Subsequently, he will do a review of the tooth to determine the condition of the piece. It may be necessary to do an x-ray and a test for pulp sensation.
Types of tooth dislocation
Tooth dislocation can range from mild to severe, on the following scale:
• Concussion: There is injury to the periodontal tissues. The tooth is loose or has moved. Often has tenderness to touch.
• Subluxation: It occurs when there is tissue injury. The tooth has not shifted from its original location but is loose and tender to the touch. There may be bleeding from the gums.
• Extrusive dislocation: The periodontal ligament is separated. The tooth has been displaced from the socket, but the socket is not affected. In these cases, the tooth looks longer than normal and is loose.
• Lateral dislocation: The alveolar bone that supports the teeth is fractured and the periodontal ligament is separated. The tooth is not loose, although it looks tilted forward or backward, relative to the gum line. When hit, it makes a high-pitched metallic sound.
• Intrusive dislocation: The tooth moves up in the alveolus, a situation that results in a fracture of the alveolar bone. The tooth is not loose. If hit, it produces a metallic sound.
Treatment and management of tooth dislocation
The procedure is required to be performed by an endodontist, a specialty that treats problems of the dental pulp and root.
The procedure to follow depends on the severity of the dislocation, as well as the part of the tooth that is injured and its magnitude. The goal of treatment is to stabilize the tooth.
Depending on the type of dislocation, different treatment options are followed:
• Concussion: A periodic review of the pulp is done for a year and does not require treatment.
• Subluxation: If there is pain when chewing, the dislocated tooth may be splinted to secure it to surrounding teeth and help stabilize it. X-rays and examinations must be done to verify the state of the pulp, for at least one year. If you want to learn more about subluxation, you can check the article here
• Extrusive dislocation: The root zone is cleaned with a saline solution and the tooth is repositioned in its place. The use of a splint may be required for approximately two weeks to stabilize the tooth. If the pulp has lesions, an endodontic procedure will be required, in which the pulp is removed. The tooth is then cleaned, before being filled and sealed.
• Lateral dislocation: The tooth is removed from the socket. Subsequently, with the help of forceps, it is relocated in the alveolus. This procedure requires the use of a flexible splint for approximately four weeks. After that time, the pulp should be followed up. Reviews will be needed at two months, at three, at six months, and at one year.
Control and follow-up consultations must continue annually for the following five years. During this follow-up period, if signs of inflammation or pulpal necrosis are recorded, root canal treatment should be performed.
• Intrusive dislocation: The tooth may be allowed to return to its original position. If this does not happen in a month, surgery will be necessary to relocate it. Another reason to perform the intervention is that the tooth has moved more than seven millimeters into the socket.
After surgery, a splint will be needed for four weeks (minimum) to support the tooth as it heals and bonds with the surrounding teeth on each side. That splint can be made of wire, metal, or resin.
If the pulp becomes inflamed or shows necrosis, endodontic treatment may be required two to four weeks after surgery. This implies carrying out controls after two months, three months, six months, and one year. Subsequently, the annual review must be done in the next five years.
Care after treatment
1. Use a soft brush after each meal.
2. Consume soft foods and liquids for a week.
3. Use antibacterial mouth language twice a day for one week.
4. As required or prescribed by the dentist, take anti-inflammatory medications.
5. Visit the dentist periodically to review the status and evolution of the dislocated tooth.
This follow-up is important to do in any type of dental dislocation.
Prompt treatment of a dislocated tooth, good oral hygiene, and regular checkups will help maintain the health of the tooth after the incident.
Nevertheless, some situations can affect the tooth that has been treated:
• Ankylosis: The tooth fuses with the bone and sinks into the gum tissue.
• Periodontitis apical: Inflammation of the tissue surrounding the tooth.
• Inflammatory root resorption: Failure or breakdown of the root structure that can cause the tooth to become loose.
• Obliteration of the pulp canal: Accumulation of calcified tissue along the entire length of the root canal, as well as on its walls. Pain is usually not felt, but it can cause pulp necrosis.
• Pulp necrosis: It is the death of the pulp, a situation in which the tooth must be removed.
Prevention
• Wear a seat belt in the car
• Wear a helmet to ride a bike
• Wear a mouth guard and a helmet when practicing rough sports.
The specialists point out that, when treating this type of trauma, the main objective is the formation of hard tissue that preserves the pulp and prevents inflammation, preserving the health and permanence of the intervened piece.
If a situation occurs that causes the dislocation of a tooth, it is advisable to consult the dentist as soon as possible and start the corresponding treatment and give you tips for the management of tooth dislocation, depending on the type of injury.
Frequently Asked Questions
How do you treat a dislocated tooth?
Current guidelines recommend repositioning a luxated tooth to its original position using digital pressure and stabilizing it for at least two weeks to promote periodontal ligament repair. Additionally, endodontic treatment with calcium hydroxide should be administered to prevent root resorption.
Can a dislodged tooth be repaired?
The dentist will secure the dislodged tooth to the adjacent teeth to hold it in place (splinting). After a couple of weeks, you will likely need to return to have the splint removed. If the tooth cannot be found or saved, it can usually be replaced with a false tooth.
How do you fix a dislodged tooth?
To fix a dislodged tooth, your dentist will first clean and numb the area. Then, they will reposition the tooth and stabilize it in the socket. Additionally, the dentist will take X-rays to assess the condition of the roots, nerves, and blood vessels for any potential damage.
Should a dislodged tooth be reinserted?
If an adult tooth is knocked out, try to reinsert it and see a dentist immediately. Do not attempt to reinsert a baby tooth; instead, take your child to a dentist right away. If you can’t reinsert the adult tooth, place it in milk and contact your dental practice promptly.
How do you save a dislodged tooth?
Treatment options usually include using a splint, wire bracket, or undergoing a root canal. An oral and dental splint helps the surrounding bone heal by securing the dislodged tooth root to the adjacent bone.
Share:
References
1. American Association of Endodontists (2014), The Treatment of Traumatic Dental Injuries / https://www.aae.org/specialty/wp-content/uploads/sites/2/2017/06/ecfe_summer2014-final.pdf
2. Cleveland Clinic (August 30, 2021),Tooth Luxation / https://my.clevelandclinic.org/health/diseases/21770-tooth-luxation
3. Dental Trauma Guide (s.f) Diagnosis of trauma: root fracture + lateral dislocation / https://dentaltraumaguide.org/es/trauma-diagnosis-rootfracture-lateralluxation/
4. Goswami, M / Rahman, B / Singh B (December 17, 2019).Outcomes of luxation injuries to primary teeth-a systematic review / National Library Of Medicine / https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7254462/
5. Medrano, Giannina / Díaz, María Elena (June 2010)Diagnosis and treatment of dental dislocations in the deciduous dentition / Revista Stomatológica Herediana, vol. 20, no. 2 / https://www.redalyc.org/pdf/4215/421539358010.pdf
6. Peralta, Alejandra / Curiel, Sergio (June 2019),Management of post-traumatic dental complication. Case report / Vital Dentistry No. 30 / https://www.scielo.sa.cr/scielo.php?script=sci_arttext&pid=S1659-07752019000100007
-
Nayibe Cubillos M. [Author]
Pharmaceutical Chemestry |Pharmaceutical Process Management | Pharmaceutical Care | Pharmaceutical Services Audit | Pharmaceutical Services Process Consulting | Content Project Manager | SEO Knowledge | Content Writer | Leadership | Scrum Master
View all posts
A healthcare writer with a solid background in pharmaceutical chemistry and a thorough understanding of Colombian regulatory processes and comprehensive sector management, she has significant experience coordinating and leading multidisciplina...