Last Updated on: 19th September 2025, 12:30 pm
Oral ulcers are a common symptom of lupus, often appearing during flares or as a side effect of medications. These mouth sores may be painless or cause burning and discomfort, especially when eating or brushing. They typically show up on the tongue, cheeks, gums, or roof of the mouth. To manage them, use saltwater rinses, topical gels, avoid irritants like spicy foods, and maintain gentle oral hygiene. See a dentist if sores last over 10 days or worsen. Tracking triggers and staying hydrated can help prevent future outbreaks and improve comfort.
Living with lupus is a daily challenge, and for many people, oral discomfort is one of the most frustrating. Oral ulcers are among the most common symptoms of lupus. While they’re usually not dangerous, they can be very uncomfortable and disruptive to everyday life.
Understanding why these ulcers appear, how to manage them, and what steps you can take to ease the discomfort is essential. In this article, you’ll find clear, practical advice to help you care for your oral health if you experience mouth ulcers in lupus.
Whether you’re newly diagnosed or have been managing lupus for years, this guide will help you take better care of your mouth and yourself.
What are oral ulcers in lupus and why do they occur?

Oral ulcers, also called mouth sores, are a common symptom in people with systemic lupus erythematosus (SLE). For many, they are a recurring part of lupus flares, periods when the disease becomes more active.
At first, these lesions may go unnoticed because they don’t always cause pain. But as they grow or become irritated, they can make everyday activities like eating, speaking, or brushing your teeth uncomfortable or even painful.
Oral ulcers are sometimes one of the first signs of a lupus flare-up. One study noted that ulcers may be more common in individuals who develop SLE during childhood, and that up to 75% of people with lupus have reduced saliva flow, a condition that can increase the risk of oral health problems like ulcers.
Why does lupus cause oral ulcers?
Mouth ulcers are a common symptom of lupus and can appear during flares or periods of remission.
- During flares, they’re caused by widespread inflammation as the immune system attacks healthy tissues, including the lining of the mouth.
- During remission, they’re often a side effect of lupus medications like corticosteroids or immunosuppressants, which can weaken oral tissues and slow healing.
In addition to disease activity and treatment, some other factors can increase the risk or worsen the severity of mouth sores:
- Stress: Physical and emotional stress can weaken the immune system and trigger flares.
- Hormonal changes: Shifts in hormones, especially around menstruation or pregnancy, can make the mouth more sensitive.
- Nutrient deficiencies: Low levels of iron, folic acid, or vitamin B12 can contribute to the appearance of ulcers.
- Dry mouth (xerostomia): This is especially common in lupus patients, particularly those with overlapping conditions like Sjögren’s Syndrome. Without enough saliva, the mouth becomes dry and irritated, making it more prone to sores and infections.
Understanding these triggers can help you and your healthcare team find ways to reduce flare-ups and manage symptoms more effectively.
Recognizing oral ulcers in lupus

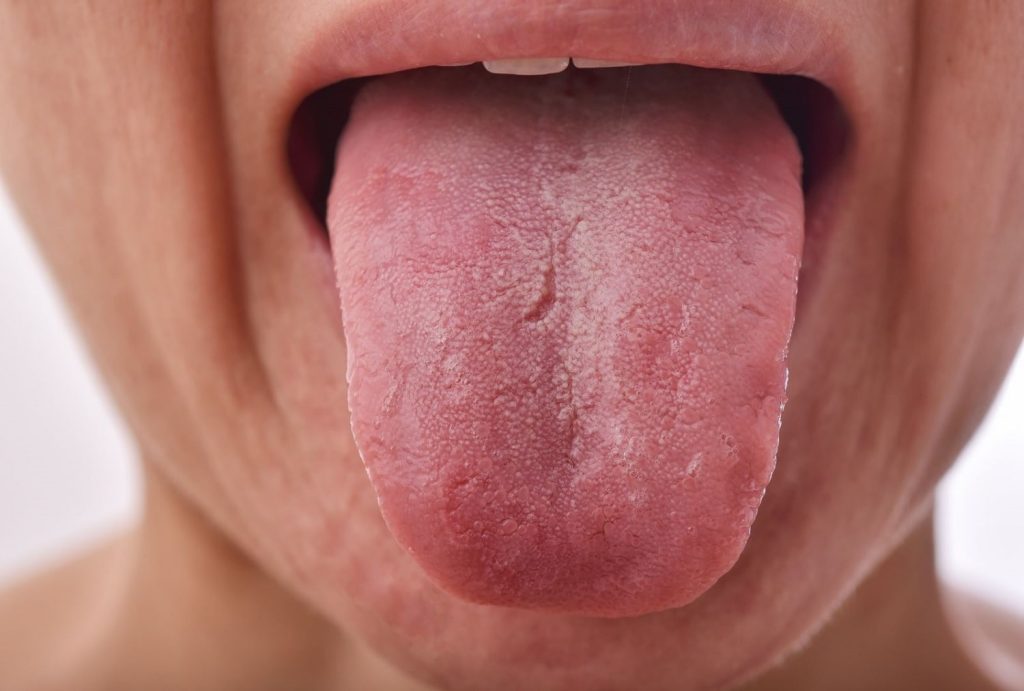
Mouth ulcers in lupus can look and feel different from person to person, but they often share common features. These sores often appear on the tongue, inner cheeks, gums, or roof of the mouth, and they can show up alone or in clusters.
Common characteristics:
- Shape: usually round or oval
- Color: often has a white or yellowish center with a red, inflamed border
- Pain: some are painless, while others can sting or burn, especially when eating spicy, salty, or acidic foods
Types of lupus mouth sores:
There are generally two types, depending on when they appear and the cause:
- Medication-related sores (outside of flares):
- often, a side effect of lupus treatments like corticosteroids or immunosuppressants
- typically appear as raised white bumps with red lines around them
- usually painless
- Flare-related sores (during active disease):
- caused by inflammation from an immune system attack
- tend to be red lesions with a white halo or white lines radiating from the center
- can be painful and more sensitive to certain foods
If you experience oral ulcers frequently, it’s a good idea to keep track of their appearance, how long they last, and any triggers like stress, diet, or hormonal changes. Sharing this information with your doctor or dentist can help them better understand your symptoms and personalize your care.
When should you see a dentist?

While some ulcers go away on their own, you shouldn’t ignore them, especially if:
- they last more than 10–14 days
- they bleed, swell, or grow rapidly
- they change in color, shape, or size
- they interfere with your ability to eat or talk comfortably
- you get them frequently
Let your dentist know you have lupus from the very first visit. This helps them provide tailored care and avoid treatments or products that could further irritate your mouth. Dentists can teach you specific brushing techniques, recommend soothing products, and help prevent complications like secondary infections.
How to treat oral ulcers from lupus?

There’s no single cure for oral ulcers in lupus, but many treatments and habits can reduce pain, speed up healing, and prevent future outbreaks. The most effective approach often combines medical treatment, home remedies, and daily oral care.
Medical treatments
These are prescribed or recommended by healthcare professionals, especially for moderate to severe ulcers:
- Topical corticosteroids: Gels or creams like hydrocortisone reduce inflammation and are often the first line of treatment.
- Oral corticosteroids or immunosuppressants: For persistent or severe ulcers, your doctor may adjust your lupus medication or prescribe systemic anti-inflammatories.
- Antimalarials: Medications like hydroxychloroquine may be used if ulcers are tied to lupus activity.
- Pain-relieving and anti-inflammatory gels: Products with benzocaine or lidocaine (e.g., Shop Orajel Here, Anbesol) help numb the area.
- Medicated mouthwashes: Including chlorhexidine or painkilling rinses to prevent infection and relieve discomfort.
- Corticosteroid lozenges: Sometimes recommended for easier application on multiple sores.
At-home remedies
You can support healing and relieve symptoms with simple care routines at home:
- Saltwater rinses: A simple mix of warm water and salt (½ teaspoon per glass) can help clean and soothe the affected area.
- Aloe vera gel: Apply a small amount of pure aloe vera directly on the sore to reduce inflammation and support healing.
- Avoid irritants: Stay away from spicy, hot, acidic, or crunchy foods that can make sores worse. Tobacco and alcohol should also be avoided.
- Moist gauze: If brushing is too painful, you can use a damp, sterile gauze to gently clean your mouth.
- Hydration: Drink plenty of water throughout the day to reduce dry mouth and support healing.
What daily habits can help protect your mouth from Lupus-Related Ulcers?

1. Gentle oral hygiene
- Brush twice a day using a soft-bristled toothbrush, like Oral-B Sensitive gum care.
- Use non-abrasive, alcohol-free toothpaste and mouthwash.
- Floss gently and regularly. (See Dental Floss Here)
- Replace your toothbrush regularly to avoid bacteria buildup.
2. Watch what you eat
- Go for bland, soft foods like mashed vegetables, oatmeal, soups, smoothies, and yogurt.
- Avoid spicy, acidic, salty, and hard foods while ulcers are active.
- Limit coffee and caffeine.
- Eliminate gum and popcorn during flare-ups.
- Increase iron, folic acid, and vitamin B12 intake to support tissue repair.
3. Manage stress
Stress can trigger lupus flares, including oral symptoms. To manage it:
- Practice deep breathing, meditation, or mindfulness
- Go for a short walk or spend time in nature
- Journal, paint, stretch, or listen to calming music
- Try gentle yoga or other relaxing activities
Oral ulcers in lupus don’t always hurt at first, but over time, they can impact your daily routine and oral health. It’s important to pay attention to them early on.
With the right treatment, consistent hygiene, and professional support, it’s possible to keep these sores under control and feel better. Taking care of your mouth is more than just comfort; it’s also an important part of managing lupus and protecting your overall well-being.
Frequently Asked Questions
Are oral ulcers in lupus contagious?
How long do lupus ulcers usually last?
Can lupus mouth sores lead to other infections?
Do I need to stop my lupus medication if I get ulcers?
What’s the difference between lupus ulcers and cold sores?
Voice and Search (Q&A)
What do lupus mouth ulcers look like?
Lupus mouth ulcers are usually round or oval with a white or yellow center and a red border. They often appear on the tongue, cheeks, gums, or roof of the mouth.
How do you treat lupus-related mouth ulcers at home?
You can rinse with saltwater, apply aloe vera gel, drink plenty of water, avoid spicy or acidic foods, and brush gently with a soft toothbrush.
When should I see a dentist for lupus mouth sores?
See a dentist if ulcers last more than two weeks, bleed, grow, change color or shape, or interfere with eating or speaking.
Share
References
1. Du, F., Qian, W., Zhang, X., Zhang, L., & Shang, J. (2023). Prevalence of oral mucosal lesions in patients with systemic Lupus Erythematosus: a systematic review and meta-analysis. BMC Oral Health, 23(1). https://doi.org/10.1186/s12903-023-03783-5
2. García, R. P., Pecci, L. M. P., & Oñate, S. R. E. (2022). Oral Manifestations of Systemic Lupus Erythematosus: A Systematic Review. International journal of environmental research and public health, 19(19), 11910. https://www.mdpi.com/1660-4601/19/19/11910
3. Mayo Clinic Staff. (2022, 21 October). Lupus. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/lupus/symptoms-causes/syc-20365789
4. Rodsaward, P., Prueksrisakul, T., Deekajorndech, T., Edwards, S. W., Beresford, M. W., & Chiewchengchol, D. (2017). Oral Ulcers in Juvenile-Onset Systemic Lupus Erythematosus: A Review of the Literature. American journal of clinical dermatology, 18(6), 755–762. https://doi.org/10.1007/s40257-017-0286-9
5. Srakocic, S. (2023, 20 January). Treating and Preventing Lupus Mouth Sores. Healthline. https://www.healthline.com/health/lupus/lupus-mouth-ulcers
- Dr. Yeidy Carolina Mesa [Author]
DDS Yeidy Carolina Mesa Passionate Dentist | Advocate for Accessible Oral Health Education Graduating from Universidad CES in 2022, I am a dedicated general dentist with a lifelong passion for helping others and making a meaningful impact in the world. My journey into dentistry began at the age of 7, inspired by my own experience with braces and overcoming a fear of the dentist. This personal journey shaped my mission to help patients conquer their own dental anxieties and embrace a healthier,...
View all posts
- Nayibe Cubillos M. [Medical Reviewer]
Pharmaceutical Chemestry |Pharmaceutical Process Management | Pharmaceutical Care | Pharmaceutical Services Audit | Pharmaceutical Services Process Consulting | Content Project Manager | SEO Knowledge | Content Writer | Leadership | Scrum Master
View all posts
A healthcare writer with a solid background in pharmaceutical chemistry and a thorough understanding of Colombian regulatory processes and comprehensive sector management, she has significant experience coordinating and leading multidisciplina...Recent Posts