Last Updated on: 12th December 2025, 10:21 am
What is peri-implantitis? How can this problem affect you? Here is a complete explanation.
Tooth loss is more common than you might think, whether due to cavities, smoking, or accidents. Fortunately, there are several solutions to restore your smile, from removable dentures to fixed options. However, dental implants stand out as the best choice, offering a natural look and function. They are durable and comfortable;with proper care, they can last a lifetime.
But implants are not risk-free. One of the most concerning issues is peri-implantitis, a gum infection that affects about 1 in 3 people with implants. This condition can lead to bone loss and, in severe cases, implant failure. Despite their high success rate, over 98%, implants require strict oral hygiene and regular checkups to prevent complications.
The good news? Peri-implantitis is preventable. If you already have implants or are considering getting one, understanding the risk factors and adopting the right care habits will help you maintain a healthy smile for years to come.
What is peri-implantitis?
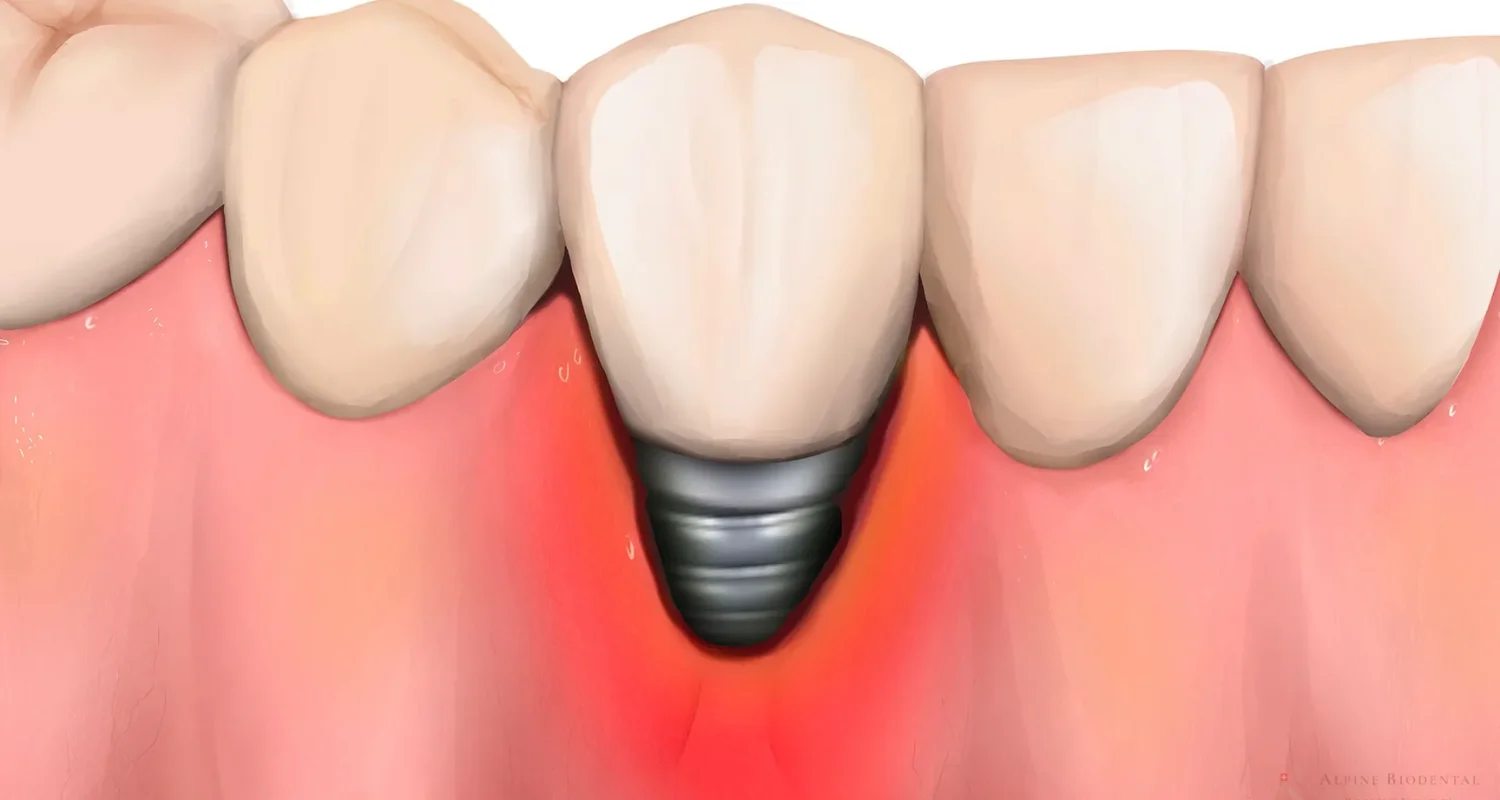
Peri-implantitis is a serious condition that affects the gum tissue and bone surrounding a dental implant. Think of it as the implant version of gum disease: it starts with inflammation and, if left untreated, can lead to bone loss and even complete implant failure. Essentially, the very foundation that holds the implant in place begins to break down, causing it to loosen and, in the worst cases, fall out.
This condition happens when bacteria build up around the implant, leading to infection. It can develop slowly over time (chronic) or appear suddenly (acute) with severe symptoms.
Symptoms of peri-implantitis
Your body gives warning signs when something is wrong with your dental implant. Recognizing these early will help prevent serious damage and even save the implant. These conditions develop in different stages:
1. Peri-implant mucositis (early stage)
This is the first and mildest stage, where the soft tissues around the implant become inflamed due to bacterial buildup. It’s reversible with proper oral care. Key symptoms include:
-Red or swollen gums around the implant.
-Bleeding when brushing or touching the area.
-Mild discomfort or tenderness in the gums.
-A bad taste in the mouth due to bacteria buildup.
With proper cleaning and professional care, peri-implant mucositis can be stopped before it progresses.
2. Peri-implantitis (moderate stage)
What is peri-implantitis? Now you know it. However, if left untreated, inflammation spreads deeper, leading to bone loss around the implant. At this stage, immediate treatment is needed to prevent further damage. Symptoms may include:
-Excessive bleeding and gum swelling around the implant.
-Deep pockets forming between the gum and implant.
-Mild to moderate bone loss, visible on X-rays.
-Pain while chewing.
Without intervention, bone deterioration will continue, increasing the risk of implant failure.
3. Peri-implant abscess (severe stage)
At this advanced stage, the infection becomes severe, and the implant is at high risk of failing. In some cases, a peri-implant abscess (a pus-filled infection) may develop. Warning signs include:
-Significant bone loss, detected through X-rays.
-Loosening of the implant due to lost support.
-Sharp pain that spreads to the jaw or upper face.
-Pus discharge from the implant site.
-Swelling in the gums and face, sometimes altering facial appearance.
-Fever, a sign of a spreading infection.
This stage requires urgent treatment to prevent further damage.
4. Implant failure
If left untreated, peri-implantitis can lead to complete implant failure. At this point, the implant must be removed, and additional procedures like bone grafting may be required before attempting a new implant.
Catching peri-implantitis in its early stages can prevent major damage and save the implant. Periodontists use X-rays and advanced diagnostic tools to monitor bone loss and plan the best treatment.
What is Peri-implantitis: How common and what puts you at risk?

Peri-implantitis is more common than most people realize. It is the number one reason implants fail, whether they’re supporting fixed crowns or implant-supported dentures. About 1 in 3 people with dental implants will develop some form of it. However, not everyone faces the same risk; certain habits, health conditions, and lifestyle choices make it more likely to develop.
What increases the risk?
Several factors can contribute to peri-implantitis, including:
● Poor oral hygiene: Not brushing and flossing properly allows bacteria and plaque to build up around the implant. Over time, this can lead to inflammation in the gums and, in severe cases, bone loss around the implant. Just like natural teeth, implants need daily care to stay in good shape. If you think this might happen to you, the next step is to have a better oral health routine. Here are our products recommendations to improve it.
● Harmful habits: Certain lifestyle choices can slow down healing and increase inflammation, making implants more vulnerable to infection. Some of the biggest culprits include:
–Smoking: Weakens the gums and reduces blood flow, making it harder for the implant to heal.
–Alcohol: Can contribute to gum irritation and increase the risk of infection.
–Drugs (like cocaine): Damage oral tissues and suppress the immune system, making it harder for the body to fight off bacteria.
● Medical conditions: Some medical conditions can slow down healing, weaken the immune system, or affect bone strength, making peri-implantitis more likely. In some cases, getting an implant is not recommended because of potential health risks. These conditions include:
-Severe heart disease.
-Autoimmune disorders.
-Blood clotting problems.
-Osteoporosis (which weakens bones).
-Hypothyroidism.
-Recent heart attack or stroke.
-A weakened immune system (due to illness or medication).
-Ongoing cancer treatment.
Even though pregnancy isn’t a disease, getting an implant while pregnant is not recommended. There’s a risk of infection, complications, and the negative effects of medication on both the mother and baby. It’s best to wait until after pregnancy to ensure a safe and smooth recovery. Also, the best way is prevet losing teeth during pregnancy.
● A history of gum disease: If you’ve had periodontal disease (gum disease) before getting an implant, you’re at a higher risk of developing peri-implantitis. Periodontal disease causes plaque buildup that weakens the bone supporting teeth. If implants are placed without addressing existing gum problems, the risk of failure is much greater.
● Excessive bite force: Implants are strong, but they have limits. If they’re exposed to too much pressure while chewing, it can weaken the connection between the implant and the bone. This is especially common in:
-People who grind their teeth (bruxism): The constant pressure can loosen the implant over time.
-Implants supporting too much force: If an implant has to handle more load than it should, it may start to move.
● Poor implant placement or technical errors: Not all implant procedures are done correctly, and mistakes can increase the risk of peri-implantitis. To avoid complications, it’s important to have implants placed by a trained specialist. Some common errors that can lead to problems include:
-Using low-quality materials or improper tools.
-Not maintaining proper sterilization during the procedure.
-Poor planning or lack of communication with the patient.
-Lack of experience from the dental professional.
● Skipping dental checkups: Regular dental checkups before and after getting an implant are essential. Your dentist can spot early signs of infection and treat them before they turn into serious problems. Skipping appointments means missing out on early detection and prevention, increasing the risk of peri-implantitis and implant failure.
By understanding these risk factors and taking preventive steps, you can protect your dental implants and ensure they last for years to come.
How to prevent peri-implantitis?

Dental implants are designed to be a long-term solution, but they require proper care to stay healthy. The best way to avoid peri-implantitis is to take care of your implants from the start. Here’s how you can protect them:
● Brush and floss daily: Clean around your implants at least three times a day and use any special tools your dentist recommends. For better clean up, you could use an interdental brushes. Hera are two options that we recommend you:
● Avoid smoking, alcohol, and drug use: These bad habits slow healing, weaken your immune system, and increase inflammation.
● Keep your body healthy: Stay hydrated, eat a balanced diet, and manage conditions like diabetes that can affect healing.
● Visit your dentist regularly: Routine checkups will help catch early signs of peri-implantitis before they become serious.
● Protect your implants from excessive force: If you grind your teeth, talk to your dentist about wearing a nightguard.
● Pay attention to warning signs: If you notice redness, swelling, or discomfort around your implant, don’t wait, see your dentist right away.
So, what is peri-implantitis? Taking care of your implants doesn’t have to be complicated and can prevent it. A little effort goes a long way in keeping them strong, secure, and problem-free for the future.
How to treat peri-implantitis
Catching peri-implantitis early is essential to prevent serious complications and save your implant. Treatment depends on how advanced the condition is and typically includes a combination of deep cleaning, antibacterial treatments, and in some cases, surgery.
Non-surgical treatment (for early stages)
What is peri-implantitis? If it is detected early, the goal is to remove bacteria and stop the infection before it spreads to the surrounding bone. Non-surgical treatments include:
● Mechanical debridement: Removal of plaque and tartar from the implant surface using ultrasonic tools, curettes, or specialized instruments.
● Antibacterial treatments: Using antimicrobial mouth rinses (like chlorhexidine) or topical antibacterial gels to control infection. In some cases, oral antibiotics may be prescribed.
● Laser therapy: Dental laser, can help disinfect the area with less trauma to surrounding tissues and reduce the need for anesthesia.
● Ozone therapy: A treatment used to kill bacteria and promote healing.
Surgical treatment (for moderate to severe cases)
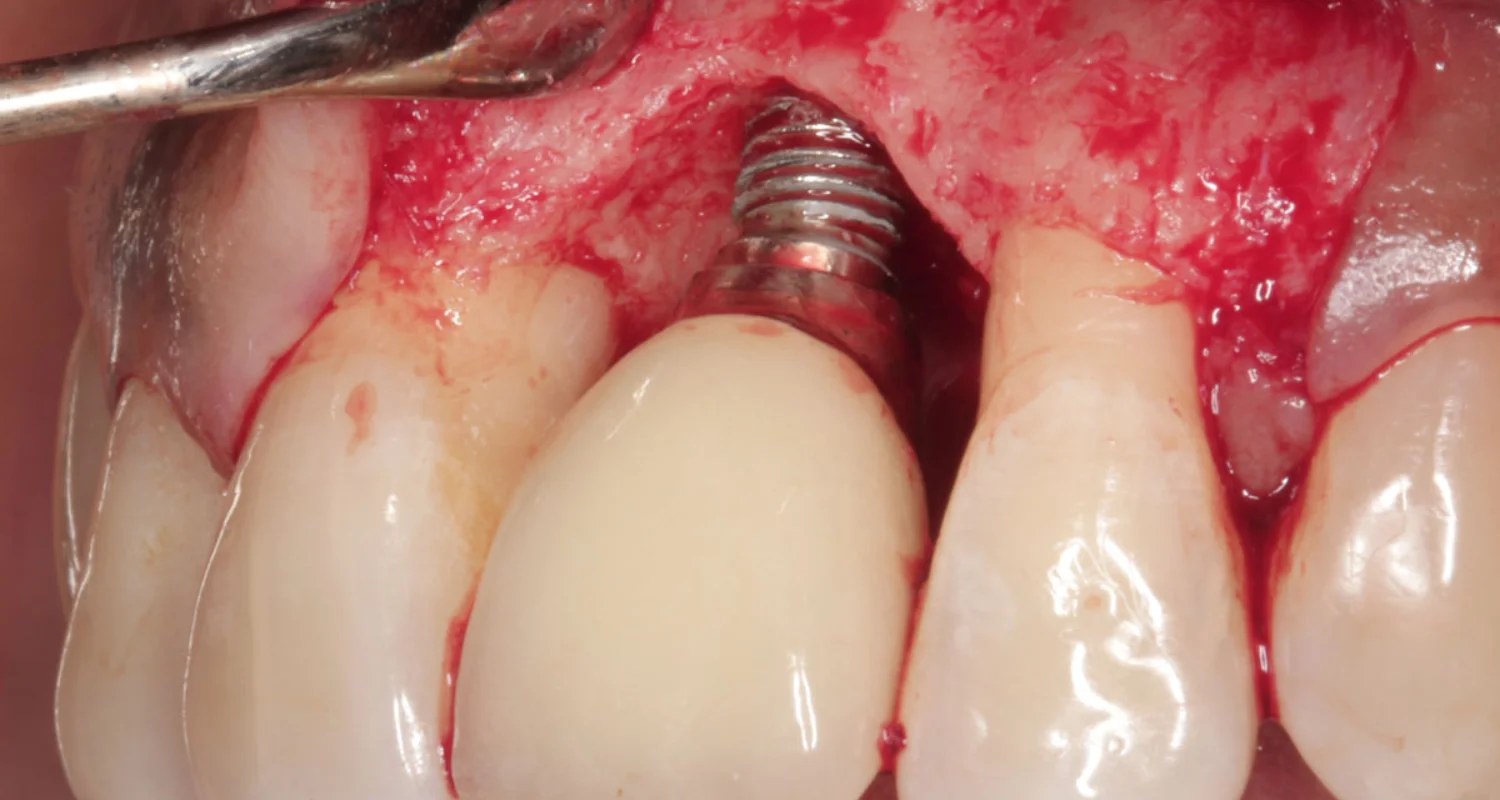
When peri-implantitis has already caused bone loss, surgery may be necessary to either save the implant or remove the infection entirely. Surgical treatments may include:
● Bone grafting and membrane placement: Used to regenerate lost bone and strengthen implant support.
● Deep implant cleaning and guided tissue regeneration to help the gums heal properly.
● Implant removal: If the infection is too advanced, removing the implant may be the best option, especially if it’s in a non-visible area like the back teeth.
At-home care (supportive treatment)
While professional treatment is needed to manage peri-implantitis, you can take steps at home to prevent further damage and support healing:
● Use specialized oral hygiene tools: Interdental brushes, water flossers, and implant-friendly toothbrushes help keep the area clean.
● Use antibacterial toothpaste and mouth rinses: especially those containing chlorhexidine or other germ-fighting agents.
● Stay consistent with your oral hygiene routine: Brush and floss daily to prevent bacterial buildup.
What is peri-implantitis? It’s an infection that affects the tissue around dental implants, and if it’s not treated in time, it can put their stability at risk. But don’t panic! Just because poor oral hygiene or health issues can increase the risk doesn’t mean you’re doomed to lose your implant. With early detection and proper treatment, the problem can be managed, keeping both your implant and oral health intact.
The secret? Prevention (and a little consistency!). Brushing and flossing daily, seeing your dentist regularly, and ditching habits like smoking are the best ways to keep your implants safe. Think of them as a long-term investment in your smile: the better you care for them, the longer they’ll last.
Frequently Asked Questions
What is peri-implantitis? Can it be reversed?
If caught early (in the mucositis stage), it can be treated and reversed with professional cleaning and better oral care. However, once bone loss occurs, treatment focuses on stopping further damage rather than fully reversing it.
Can peri-implantitis spread to other teeth?
Yes, if left untreated, the bacteria causing peri-implantitis can spread to nearby gums and natural teeth, increasing the risk of gum disease (periodontitis) and further infections.
Are some types of implants more resistant to peri-implantitis?
Some studies suggest that titanium implants with special coatings may be more resistant to bacterial buildup. However, proper care and regular cleanings are more important than implant type.
Are people with weak immune systems more at risk?
Absolutely. People with conditions like HIV, autoimmune diseases, or those undergoing chemotherapy are at higher risk because their bodies struggle to fight infections.
Who is more at risk for peri-implantitis: men or women?
There’s no clear difference between men and women in terms of peri-implantitis risk. It’s more about individual factors like oral hygiene, smoking, health conditions (like diabetes), and a history of gum disease.
Men who smoke may have a higher risk, while postmenopausal women with osteoporosis may also be more vulnerable due to lower bone density. In the end, lifestyle and health habits matter more than gender.
Share
References
1. AAP. (2019, 21 Jun). Peri-Implant Diseases – American Academy of Periodontology. American Academy Of Periodontology. https://www.perio.org/for-patients/periodontal-treatments-and-procedures/dental-implant-procedures/peri-implant-diseases/
2. Assery, N. M., Jurado, C. A., Assery, M. K., & Afrashtehfar, K. I. (2023). Peri-implantitis and systemic inflammation: A critical update. The Saudi Dental Journal, 35(5), 443-450. https://doi.org/10.1016/j.sdentj.2023.04.005
3. Berglundh, T., Mombelli, A., Schwarz, F., & Derks, J. (2024, 2 February). Etiology, pathogenesis and treatment of peri‐implantitis: A European perspective. Periodontology 2000. https://doi.org/10.1111/prd.12549
4. Gurarie, M. (2024, 23 Oct). 9 Common Causes of Bad Dental Implants. Verywell Health. https://www.verywellhealth.com/dental-implant-failure-5217573
5. Heitz, M. L. (2024). Peri-implant mucositis and peri-implantitis: key features and differences. Br Dent J 236, 791–794. https://doi.org/10.1038/s41415-024-7402-z
6. Mayo clinic collaborators. (2019, 29 January). Dental implant surgery. Mayo Clinic. https://www.mayoclinic.org/tests-procedures/dental-implant-surgery/about/pac-20384622
7. Roccuzzo, M., Mirra, D., & Roccuzzo, A. (2024). Surgical treatment of peri-implantitis. BDJ, 236(10), 803-808. https://doi.org/10.1038/s41415-024-7405-9
- DDS Juliana Garzon [Author]
Dr. Juliana Garzón Ariza Endodontics Specialist | Passionate Advocate for Oral Health Transformation Graduating from the esteemed Universidad Nacional de Colombia in 2021, I am a dentist and a final-year resident specializing in Endodontics. My professional mission is to transform oral health through prevention, highly specialized treatments, and patient education. With a strong focus on dental research, I am driven to innovate solutions in critical areas such as dental pain, infections, dent...
View all posts
- Dr. Yeidy Carolina Mesa [Medical Reviewer]
DDS Yeidy Carolina Mesa Passionate Dentist | Advocate for Accessible Oral Health Education Graduating from Universidad CES in 2022, I am a dedicated general dentist with a lifelong passion for helping others and making a meaningful impact in the world. My journey into dentistry began at the age of 7, inspired by my own experience with braces and overcoming a fear of the dentist. This personal journey shaped my mission to help patients conquer their own dental anxieties and embrace a healthier,...
View all posts