Last Updated on: 16th December 2025, 10:59 am
Have you ever felt a sharp or intense pain in your gums near a tooth that is trying to emerge? If so, you might be dealing with a case of pericoronitis. And, in that case, you might be looking for a pericoronitis treatment at home.
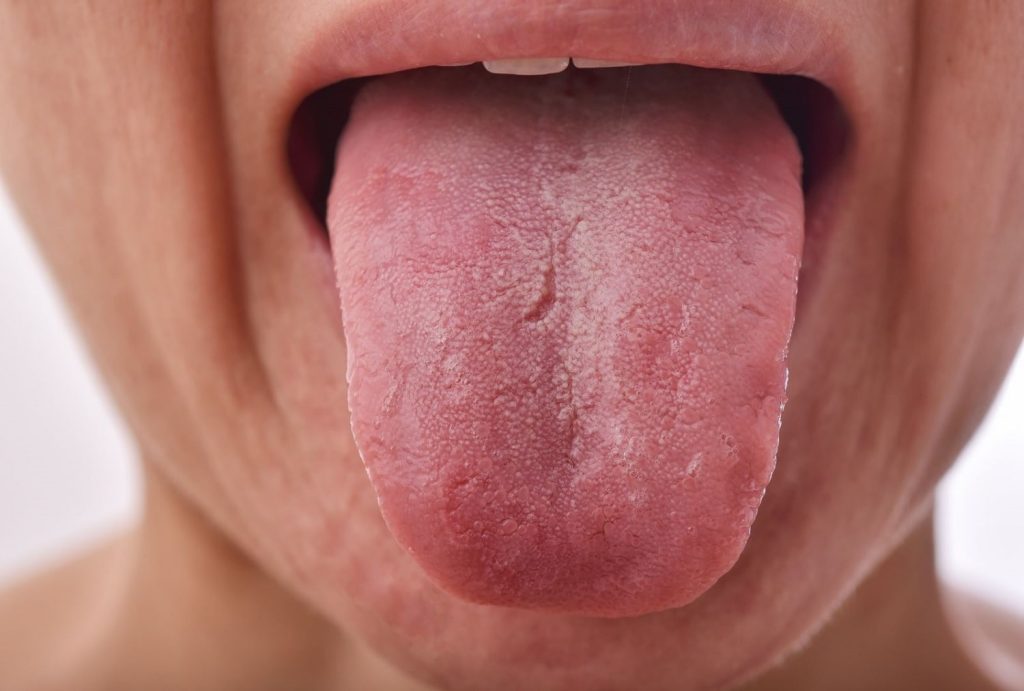
Pericoronitis is a common dental condition, often associated with partially erupted wisdom teeth. It occurs when the gums surrounding a tooth that has not fully erupted become inflamed or infected, typically due to trapped food debris and bacteria.
This condition may start with mild discomfort but, if left untreated, it can become very painful and disrupt daily activities such as eating, speaking, or even sleeping. This article explores effective pericoronitis treatment at home while providing a detailed overview of its causes, symptoms, and preventive measures. Additionally, we’ll discuss the signs that indicate when it’s time to seek professional dental care.
What is Pericoronitis?

Before a tooth emerges, it develops beneath the gum tissue, waiting for the appropriate time to break through. As it begins to erupt, the tooth pushes upward, gradually forcing the gum to open and make way for its emergence. However, in some instances, the gum does not completely separate, leaving the tooth only partially exposed. This condition, known as partial eruption, results in part of the tooth being visible while the rest remains covered by a flap of gum tissue.
Pericoronitis refers to the inflammation of the gum tissue surrounding a tooth that has not fully erupted. It most commonly affects wisdom teeth, especially those in the lower jaw. This is because the lower wisdom teeth often face challenges during eruption due to limited space in the mouth, which can cause them to become partially exposed or trapped under the gum. This partial eruption creates an environment where bacteria and debris can accumulate, leading to irritation, swelling, and infection in the surrounding gum tissue.
Who Suffers From Pericoronitis?
Pericoronitis can affect anyone; however, it is more common in teenagers and young adults, usually between the ages of 17 and 25, the time when wisdom teeth begin to emerge.
Causes
Some of the most common causes include:
● Bacterial accumulation: Food debris trapped under the gum covering the tooth can promote bacterial growth.
● Partially erupted teeth: When a tooth doesn’t fully emerge, it can rub against or put pressure on the surrounding gums.
● Gum overload: The tissue partially covering the tooth may be subjected to excessive pressure during chewing or as the tooth tries to emerge.
Risk factors
Several factors can increase the chances of developing pericoronitis. They may act on their own or work together to raise the risk:
● Poor oral hygiene: If the mouth is not kept clean, food particles and bacteria can accumulate around partially erupted wisdom teeth, creating a breeding ground for infection and inflammation in the gums.
● Lack of space in the jaw for wisdom teeth: When there is insufficient space for the wisdom teeth to emerge properly, they may become impacted or partially erupt, leading to gum irritation, infection, and pericoronitis.
● Inflamed or sensitive gums due to partially erupted teeth: When a tooth doesn’t fully erupt, it can cause the gum tissue around it to become irritated and inflamed. This can make the gum more vulnerable to infection, leading to pericoronitis.
Common Signs and Symptoms of Pericoronitis

● Intense and localized pain: This pain typically occurs in the gum tissue around the affected tooth, and it can be sharp or throbbing.
● Swelling, redness, and inflammation of the gums: The gums surrounding the affected tooth become swollen and may appear redder than usual due to irritation and infection.
● Pus or discharge: If the infection becomes more severe, pus may start to drain from the gum area near the tooth, indicating an ongoing infection.
● Bad breath or unpleasant taste: The accumulation of bacteria, food debris, and pus in the infected area can lead to foul-smelling breath or an unpleasant taste in the mouth.
● Difficulty opening the mouth (trismus): Swelling and pain from the infection can cause the muscles and tissues around the jaw to become stiff, making it harder to open the mouth fully. This can affect eating and speaking.
It is important to see a dentist if the symptoms do not improve within a few days if the pain increases, or if signs of infection appear, such as fever or difficulty opening the mouth.
Professional Treatments for Pericoronitis
The duration of pericoronitis varies depending on how severe the case is and the treatment received. In mild cases, where good pericoronitis treatment at home care is followed, the symptoms often improve within a few days, usually between 3 and 7 days. However, in more severe cases, the condition can last for several weeks and typically requires professional dental intervention.
● Deep cleaning around the affected tooth: A thorough cleaning performed by a dentist will help eliminate food particles, plaque, and bacteria that may be trapped around the partially erupted tooth, which can help reduce inflammation and prevent infection.
● Operculectomy: It is a surgical procedure that involves removing the gum tissue partially covering the affected tooth, relieving irritation and infection, and reducing the chances of pericoronitis recurring.
● Antibiotics to manage severe infection: If the infection is significant, antibiotics may be prescribed to help fight the bacteria and prevent the infection from spreading.
● Tooth extraction for recurrent pericoronitis: In cases where pericoronitis keeps coming back, removing the wisdom tooth may be recommended to prevent further issues.
With the right treatment, complications can be avoided, and recovery is usually faster.
Best Pericoronitis Treatment at Home

If you think you might have pericoronitis, it’s crucial to visit your dentist promptly. They can assess your situation and provide the best treatment plan tailored to your needs. In the meantime, your dentist might recommend simple pericoronitis treatment at home to help ease the discomfort while you wait for professional care or during your treatment.
Natural remedies
Saltwater rinse
● Benefits: Reduces inflammation and keeps the area clean.
● Instructions: Dissolve 1 teaspoon of salt in a glass of warm water. Rinse your mouth with the solution for about 30 seconds and spit it out. Repeat 2–3 times daily, particularly after eating.
● Precautions: Ensure the water isn’t too hot, to avoid irritating sensitive gums.
Hydrogen peroxide rinse
● Benefits: Cleanses the area by killing bacteria and reducing infection.
● Instructions: Mix equal parts hydrogen peroxide and water. Swish the mixture gently in your mouth for 30 seconds, then spit it out. Use this once a day.
● Precautions: Avoid swallowing the rinse, and limit usage to prevent gum irritation.
Cold compress
● Benefits: Reduces swelling and soothes pain.
● Instructions: Wrap an ice pack or frozen vegetables in a clean cloth and apply it to the outside of your cheek near the affected area. Hold for 10–15 minutes, and repeat as needed throughout the day.
● Precautions: Never apply ice directly to your skin to prevent frostbite.
Clove oil
● Benefits: Works as a natural painkiller and fights bacteria.
● Instructions: Dab a small amount of clove oil onto a cotton swab and apply it to the inflamed gums. Leave it on for a few minutes, then rinse your mouth with warm water. You can do this once or twice daily.
● Precautions: Clove oil can be potent, so use only a small amount to avoid irritation.
Turmeric paste
● Benefits: the anti-inflammatory properties help ease pain and swelling.
● Instructions: Mix 1 teaspoon of turmeric powder with a little water to make a paste. Apply it to the swollen gum and leave it on for 5–10 minutes before rinsing with warm water. Use up to twice daily.
● Precautions: Turmeric can temporarily stain your teeth or gums, so rinse thoroughly after application.

Over-the-counter options
Ibuprofen or acetaminophen
● Benefits: Effective for managing pain and reducing inflammation.
● Instructions: Take as directed on the packaging, ensuring you do not exceed the recommended dosage.
● Precautions: If you have any medical conditions or are taking other medications, consult a doctor before using these pain relievers.
Antibacterial mouthwashes
● Benefits: Assists in eliminating bacteria and calming gum irritation.
● Instructions: Use twice daily, swishing the mouthwash gently for about 30 seconds, as recommended by your dentist or the product label.
● Precautions: Do not swallow the mouthwash and avoid excessive use, as some products may disrupt the natural balance of bacteria in the mouth.
If pericoronitis treatment at home doesn’t help relieve the pain or symptoms, it’s important to visit a dentist. You should seek professional help if the pain, swelling, or other symptoms persist for several days, or if you develop a fever or have trouble swallowing. The dentist may suggest further treatments like a professional cleaning to remove food debris and bacteria from the affected area. If pericoronitis keeps recurring, tooth extraction might be recommended to avoid future issues.
The best way to prevent pericoronitis

● Maintain good oral hygiene
Brush your teeth at least twice a day and floss to remove food particles and plaque, especially in hard-to-reach areas.
● Use antibacterial mouthwashes
Mouthwashes with antibacterial properties help reduce the buildup of bacteria, particularly around partially erupted teeth.
● Regular dental check-ups
Visiting the dentist regularly helps monitor the condition of partially erupted teeth and catch potential issues before they become complications.
● Avoid irritating the gums
Be cautious when chewing and avoid hard, crunchy, or sticky foods that could damage or irritate the gum tissue around the wisdom teeth.
Conclusion
Pericoronitis is a common condition, particularly around wisdom teeth, that can start with mild discomfort but potentially lead to more severe issues if left untreated.
While pericoronitis treatment at home, like warm salt water rinses, maintaining good oral hygiene, and using pain relievers can offer temporary relief, they are not a substitute for professional dental care. Seeking professional treatment is crucial to avoid more serious complications and to effectively address the root cause of the condition.
Frequently Asked Questions
What is pericoronitis?
Pericoronitis is an inflammation of the gum tissue surrounding a partially erupted tooth, most commonly wisdom teeth.
Can pericoronitis heal on its own?
In mild cases, pericoronitis symptoms may improve temporarily with good oral hygiene and home remedies, such as rinsing with salt water or using over-the-counter pain relievers. However, the condition often recurs if the underlying issue, such as a partially erupted tooth, is not addressed. It’s important to consult a dentist to prevent complications or long-term problems..
How long does pericoronitis last?
The duration of pericoronitis can vary, depending on its severity. Mild cases often resolve within a few days to a week with proper home care and oral hygiene. However, severe or persistent cases can last several weeks and typically require professional dental treatment to fully heal.
When should I see a dentist for pericoronitis?
You should consult a dentist if symptoms persist beyond a few days, worsen, or if you experience fever, difficulty swallowing, or severe pain.
What professional treatments are available for pericoronitis?
Treatments may include professional cleaning around the affected tooth, antibiotics for infections, operculectomy (removal of the gum flap), or tooth extraction if the condition is recurrent.
Share
References
1. Christiansen, S. (2024, 23 mayo). Pericoronitis: Severity, Home Remedies, Prevention, and More. Verywell Health. https://www.verywellhealth.com/pericoronitis-4777193
2. Gotter, A. (2018, 3 septiembre). Recognizing the Symptoms of Pericoronitis. Healthline. https://www.healthline.com/health/pericoronitis
3. Schmidt, J., Kunderova, M., Pilbauerova, N., Kapitan, M. (2021). A Review of Evidence-Based Recommendations for Pericoronitis Management and a Systematic Review of Antibiotic Prescribing for Pericoronitis among Dentists: Inappropriate Pericoronitis Treatment Is a Critical Factor of Antibiotic Overuse in Dentistry. International journal of environmental research and public health, 18(13), 6796. https://doi.org/10.3390/ijerph18136796
4. Seymour, T. (2023, 20 julio). What causes pericoronitis? https://www.medicalnewstoday.com/articles/320552
5. WebMD Editorials. (2023b, marzo 30). Pericoronitis. WebMD. https://www.webmd.com/oral-health/pericoronitis
- Dr. Yeidy Carolina Mesa [Author]
DDS Yeidy Carolina Mesa Passionate Dentist | Advocate for Accessible Oral Health Education Graduating from Universidad CES in 2022, I am a dedicated general dentist with a lifelong passion for helping others and making a meaningful impact in the world. My journey into dentistry began at the age of 7, inspired by my own experience with braces and overcoming a fear of the dentist. This personal journey shaped my mission to help patients conquer their own dental anxieties and embrace a healthier,...
View all posts