Last Updated on: 11th December 2025, 10:43 am
Hepatitis can affect oral health by causing dry mouth, gum bleeding, oral lesions, and delayed healing. These issues may result from the disease itself or its treatments. Understanding this link helps patients receive safe and effective dental care tailored to their particular condition.
Hepatitis primarily affects the liver, but it can also lead to significant changes in your oral health. People with hepatitis may experience dry mouth, bleeding, inflammation, or oral lesions, often due to a weakened immune system or medication side effects.
Understanding the connection between hepatitis and oral health helps patients and dental professionals manage both conditions safely and effectively.
What is Hepatitis?
Hepatitis is an inflammation of the liver, a vital organ responsible for filtering toxins, aiding digestion, and regulating metabolism. This inflammation can be triggered by viruses, alcohol, certain medications, autoimmune disorders, or exposure to toxins.
It can be:
- Acute: develops suddenly and resolves within six months.
- Chronic: lasts longer than six months and may lead to serious complications like cirrhosis, liver failure, or liver cancer.
According to the World Health Organization (WHO), over 350 million people worldwide live with chronic hepatitis.
What are the different types of hepatitis?
Hepatitis can be caused by different factors. Understanding the differences ensures proper care, especially when planning dental or medical treatment. Let’s discuss the main types.
What is viral hepatitis?
Viral hepatitis is the most common form caused by five main viruses: A, B, C, D, and E.
Hepatitis A (HAV)
- Spread by: contaminated food or water.
- Type: always acute.
- Outcome: usually clears on its own.
- Vaccine: yes.
Hepatitis B (HBV)
- Spread by: blood, saliva, sex, shared needles, or childbirth.
- Type: acute or chronic.
- Risks: may lead to liver damage or cancer.
- Vaccine: yes.
Hepatitis C (HCV)
- Spread by: blood (e.g., sharing needles, old transfusions).
- Type: often becomes chronic.
- Risks: high risk of cirrhosis and liver failure.
- Vaccine: no, but it can be cured with treatment.
Hepatitis D (HDV)
- Spread by: blood, but only occurs if you already have hepatitis B.
- Risks: increases severity of liver disease.
- Vaccine: no, but prevented by the hepatitis B vaccine.
Hepatitis E (HEV)
- Spread by: contaminated water.
- Type: mostly acute.
- Risks: dangerous in pregnancy.
- Vaccine: available in some countries, not widespread.
What is toxic hepatitis?

Toxic hepatitis happens when the liver reacts to harmful substances like:
- alcohol
- certain medications (e.g., acetaminophen, antibiotics)
- chemicals (solvents, pesticides, industrial fumes)
It can be acute or chronic depending upon the exposure. But, stopping the toxic substance early can prevent serious liver damage.
What is autoimmune hepatitis?
Autoimmune hepatitis is a chronic condition, where the immune system attacks your liver by mistake.
- Who’s affected: more common in women.
- Symptoms: fatigue, joint pain, and liver inflammation.
- Risks: may lead to cirrhosis if untreated.
- Treatment: managed with immunosuppressive medications like corticosteroids.
How does hepatitis affect oral health?

People with hepatitis experience different mouth symptoms. These can be caused directly by the illness or by side effects of medication; problems like weakening your immune system, a reduction of saliva flow, or slow healing are frequent.
Let’s look at the most common signs.
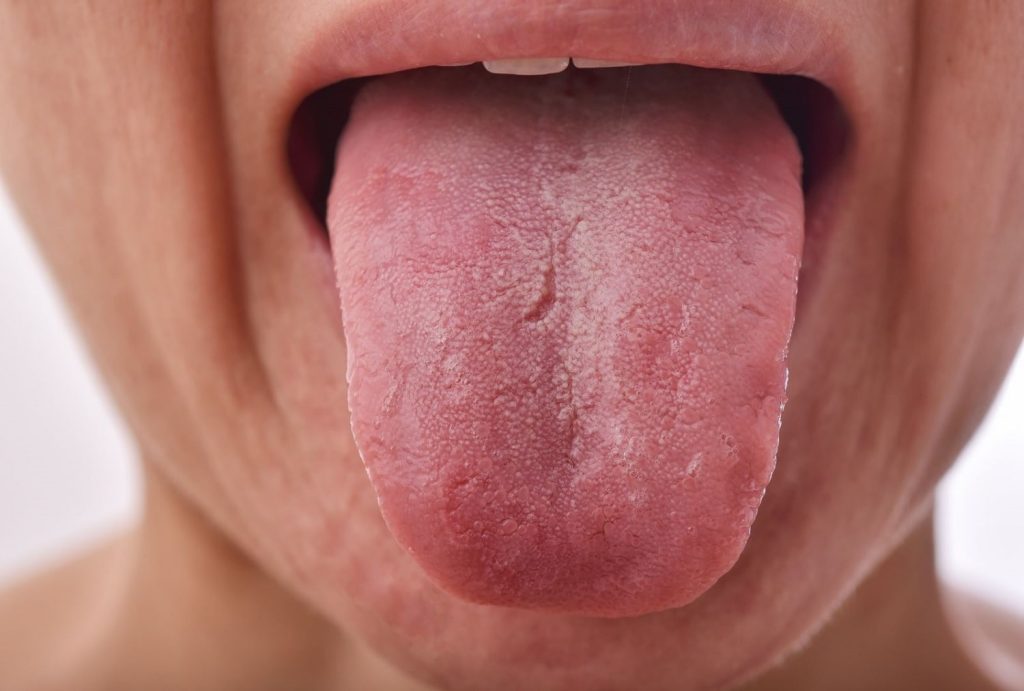
What mouth changes might I see with hepatitis?
- White or red patches (oral lichen planus): These appear as lace-like white or red patterns on your cheeks, gums, or tongue. They may hurt or itch and are more frequent in hepatitis C patients.
- Yellowish color inside the mouth (oral jaundice): Severe liver disease can cause a yellow tint inside your mouth, especially on your tongue or inner cheeks.
How does hepatitis affect saliva and mouth moisture?
- Dry mouth (xerostomia): You may feel your mouth is dry, sticky, or burning. This can make speaking, eating, and tasting difficult. Dry mouth often happens because of medications or changes in your body caused by hepatitis.
- Swollen salivary glands (sialadenitis): inflammation of the glands near your jaw or ears can cause swelling and pain, reducing saliva production.
When saliva production is reduced, teeth are more prone to develop cavities.
What types of mouth sores or gum problems are common?

- Mouth ulcers and sores: Painful small wounds can appear on your gums, tongue, or cheeks, especially when the immune system is weak.
- Gum disease (gingivitis or periodontitis): Hepatitis B and C can increase the risk of inflamed, bleeding, or swollen gums. If untreated, this may lead to tooth loss and affect overall health.
- Bleeding gums and red spots (petechiae): Liver damage can reduce clotting factors, causing easy bleeding during brushing or small red spots inside your mouth.
Why do hepatitis patients have more oral infections and healing issues?
- Fungal infections: Dry mouth and a weakened immune system increase the chances of infections like oral thrush, which looks like a white coating in the mouth.
- Slower healing after dental work: If your liver is damaged, your mouth may heal more slowly after cleanings, fillings, or extractions.
If you have hepatitis, your dentist needs to know it. This allows them to carefully plan your treatment based on your condition.
What should you tell your dentist if you have hepatitis?

Always inform your dentist about your hepatitis diagnosis, even if it’s inactive. This helps them to provide safe and personalized care. You should:
- Share details about your liver condition and any medications you’re taking.
- Bring a medical clearance or recent blood tests if your liver function is compromised.
- Tell them if you’ve had side effects like dry mouth, bleeding gums, or oral sores.
How do dentists treat hepatitis patients safely?
Dentists follow special steps to make sure your care is safe and effective:
- Coordinate with your physician to understand your liver health.
- Postpone non-urgent care if your hepatitis is active.
- Use universal precautions to prevent transmission (gloves, masks, sterilized tools).
- Monitor for medication side effects that affect the mouth.
- Offer gentle dental cleanings and recommend at-home care that won’t irritate your mouth.
What happens during a dental visit for someone with hepatitis?
Dental care is completely safe for hepatitis patients when done properly. Here’s what to expect:
- Your dentist may ask for blood test results to check your liver function.
- Urgent care (like treating infections or pain) is always prioritized.
- Non-urgent treatments are scheduled when your liver is stable.
- Your dental team will follow strict infection control, just like with any patient.
If you feel nervous, don’t hesitate to ask questions. Your dentist is trained to keep both you and the team safe.
How should hepatitis patients take care of their oral health?

If you have hepatitis, protecting your mouth is part of protecting your overall health. Here’s how you can take care of your teeth and gums every day:
- Brush gently twice a day with a soft-bristled toothbrush and fluoride toothpaste.
- Floss once a day to clean between teeth.
- Use an alcohol-free antimicrobial mouthwash, such as Crest Pro-Health, to reduce bacteria.
- Stay hydrated by drinking plenty of water throughout the day. A dry mouth can lead to decay.
- Avoid alcohol and tobacco, as they increase liver stress and dry the mouth.
- Eat a liver-friendly diet, rich in vegetables, fruits, whole grains, and lean proteins. Avoid sugary snacks and soft drinks.
Choose toothpaste and mouthwash labeled “gentle” or “sensitive” if you experience mouth soreness due to medications.
What oral care products can help hepatitis patients at home?
People with hepatitis may have dry mouth, sore gums, or higher risk of infections. Here are some helpful and easy-to-find items:
- Soft toothbrush: Colgate Gum Health is gentle on sensitive mouths.
- Fluoride toothpaste: Try Sensodyne Pronamel for enamel protection.
- Alcohol-free mouthwash: Crest Pro-Health Advanced helps fight plaque without drying.
- Dry mouth spray: Biotene Moisturizing Spray gives fast relief if you have dry mouth.
- Sugar-free lozenges: ACT Dry Mouth Lozenges can boost saliva naturally.
What should you remember about hepatitis and oral health?
Hepatitis and oral health are closely connected. When your liver is affected, your mouth may be more vulnerable to infections, dry mouth, or bleeding gums. With the right dental care and good hygiene habits at home, you can protect your overall health.
Always inform your dentist about your hepatitis status, follow all medical recommendations, and keep up with regular checkups. Taking small steps daily, like brushing, flossing, and staying hydrated, can be very helpful.
With teamwork between you and your dental team, your oral health doesn’t have to suffer.
Frequently Asked Questions
How does hepatitis influence dental procedures?
Is it possible for a dentist with hepatitis to practice his profession?
How does hepatitis impact oral health?
Is it possible to transmit hepatitis through the mouth?
Are people with hepatitis more sensitive to dental procedures?
What precautions do dentists take for patients with hepatitis?
Dentists use gloves, masks, sterilize instruments, and follow strict infection control to protect both patients and staff from hepatitis transmission.
Can hepatitis medications harm oral health?
Some hepatitis treatments can cause dry mouth or mouth sores as side effects; patients should discuss any oral symptoms with their healthcare providers.
Can I get dental treatments if I have active hepatitis?
Only emergency treatments should be done during active hepatitis; other procedures should wait until recovery.
Share:
References
1. Åberg, F., & Helenius-Hietala, J. (2022). Oral Health and Liver Disease: Bidirectional Associations, A Narrative Review. Dentistry Journal, 10(2), 16. https://doi.org/10.3390/dj10020016
2. ADA. (2022, April 1). Hepatitis viruses. American Dental Association. https://www.ada.org/resources/ada-library/oral-health-topics/hepatitis-viruses
3. Gheorghe, D. N., Bennardo, F., Popescu, D. M., Nicolae, F. M., Ionele, C. M., Boldeanu, M. V., Camen, A., Rogoveanu, I., & Surlin, P. (2022). Oral and periodontal implications of hepatitis type B and D. Current state of knowledge and future perspectives. Journal of Personalized Medicine, 12(10), 1580. https://www.mdpi.com/2075-4426/12/10/1580
4. Sheikh, A. N., Siddiquee, B., & Chahande, J. (2022). Hepatitis B and C infection among dentists – Risk, prevention, and management. Journal of Advances in Dental Practice and Research, 1, 31–36. https://doi.org/10.25259/jadpr_15_2022
5. WHO. (2024, April 9). Hepatitis B. https://www.who.int/es/news-room/fact-sheets/detail/hepatitis-b
- Nayibe Cubillos M. [Author]
Pharmaceutical Chemestry |Pharmaceutical Process Management | Pharmaceutical Care | Pharmaceutical Services Audit | Pharmaceutical Services Process Consulting | Content Project Manager | SEO Knowledge | Content Writer | Leadership | Scrum Master
View all posts
A healthcare writer with a solid background in pharmaceutical chemistry and a thorough understanding of Colombian regulatory processes and comprehensive sector management, she has significant experience coordinating and leading multidisciplina...Recent Posts