Last Updated on: 10th December 2025, 06:49 am
Dealing with dental treatment in children with autism? Difficulties in social communication and thought patterns, as well as restricted or repetitive behavior patterns, are typical of people living with autism spectrum disorder (ASD). It is estimated that by the year 2022, 80 out of every 10,000 children will be diagnosed with autism spectrum disorder in the United States.
People with ASD often have problems interacting with others, as well as different ways of learning, behaving, moving, or paying attention. All of the above makes everyday situations, such as visits to the dentist, challenging for those living with autism.
What Effects does Autism have on Oral Health?

Although autism does not involve abnormalities that directly cause oral disease, autistic people are often more prone to it than other patients of similar ages. The following conditions predispose to the development of oral pathologies in patients with ADD:
1. Tendency to self-harm
This can lead to actions such as injuring the gums, biting the lips, or causing ulcerations through self-flagellation.
2. Oral hygiene problems
For people with autism, dental hygiene can be uncomfortable, because they are often bothered by feeling wet, or the taste of toothpaste is unpleasant. Not maintaining proper oral hygiene can contribute to the development of oral diseases, such as gingivitis and tooth decay.
3. Medication Side Effects
Some medications frequently used in autistic patients can cause enlargement of the gums, known as gingival hyperplasia.
4. Difficulties in consultations with the dentist
The visit to the dental office can be a challenging event for an autistic patient, which is why many do not attend dental check-ups and routine cleanings often enough.
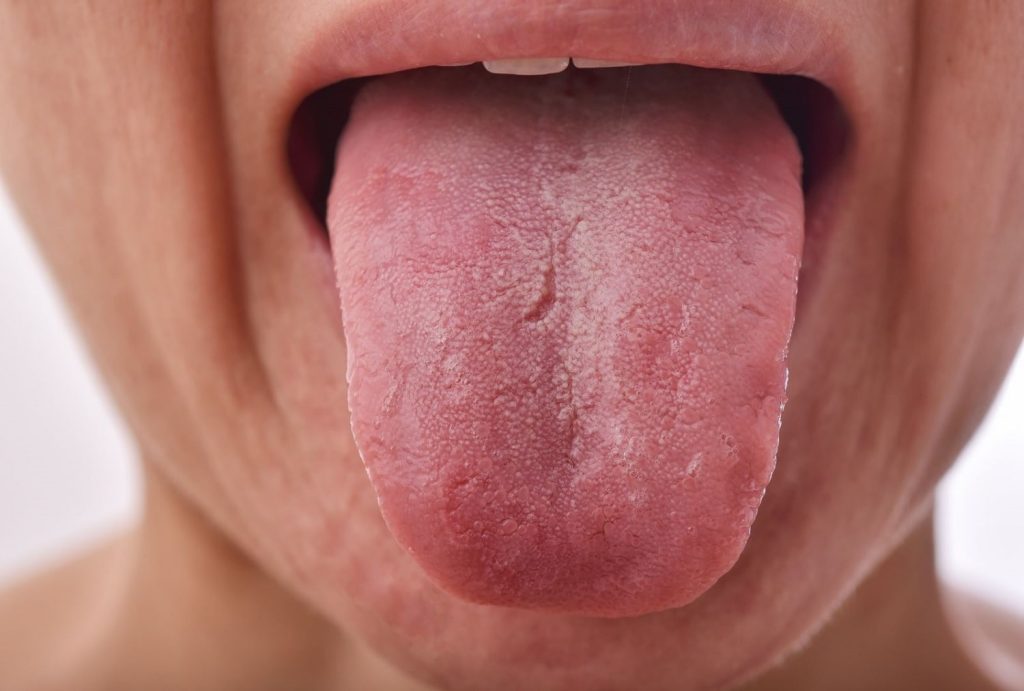
5. Harmful oral habits
Children with autism typically prefer soft, sweetened foods and tend to keep food in their mouths rather than swallow. This is a consequence of poor coordination with the tongue and significantly increases the risk of developing cavities and gum disease.
How to Prepare your Child for a Visit to the Dentist?
The following strategies can greatly improve a child’s dental office experience:
1. Previous meeting with the dental team: Meet with the dentist and his or her staff to discuss previous dental treatments and possible sensory triggers.
2. Communication with the dentist: Provide clear and sufficient information to the dentist about the patient’s medical and dental history, associated conditions, oral hygiene habits, and inappropriate behaviors
3. Desensitization appointment: Let the child become familiar with the place before undergoing treatment
4. Motivation: Do not treat a visit to the dentist as a negative or undesirable experience. Instead, helps build trust in the dental professional.
Tips for the Time of Consultation:
Carry a favorite item
Children with autism may feel more secure and calm with comforting objects, such as stuffed animals or blankets. They should stay on their lap and not get close to the face, for safety reasons during treatment.
Use of glasses
Many children can be sensitive to light, so wearing glasses can protect them from the glare of the lamps used in the office.
Use of headphones
Depending upon the preference of the child, headphones can be used to reduce the perception of noise or to listen to music. This can distract them from loud noises.
How to Find the Right Dental Treatment in Children with Autism?
A dental visit can be stressful for most people, and even more so for patients with autism. A dental checkup or procedure can involve many new sounds, tastes, and smells, which can create an overwhelming environment for patients with autism.
For a child with autism, it can be intolerable to have instruments put in their mouths. They don’t like the sensation of having a wet face or the unpleasant taste of products used during the procedures. A good way to reduce stress is to explain to the child what happens during a consultation.
Because the care of a patient with autism usually requires some considerations to make the dental practice friendly and tolerable, some dentists receive special training. These professionals usually have the following skills:

• Special communication skills
• Special oral health conditions in autistic patients
• Empathy-based dental care
• Strategies for adaptation to treatment
Oral Care in People with Autism
Knowing the challenges that dental care represents in patients with ASD is essential to adopting strategies that improve the dental experience. The following tips can facilitate and improve oral hygiene practices:

Adapt brushing to your needs
Select the type of toothbrush and accessories that best suit the needs of the child. This may include soft or specialty bristle brushes, brush handle adapters, or any other option that makes brushing easier.
Use of pictograms
If the child can brush himself, it is important to teach him to do it correctly using various techniques, such as pictograms or other visual tools that help him understand and follow instructions. It may be helpful to post these aids in a visible place so the child can routinely follow directions.
Try different flavors of toothpaste
Many children with autism prefer unflavored, non-foaming toothpaste. Explore kid-friendly flavored toothpaste options to find the most suitable and palatable for your child.
Flavored dental floss
Some children with autism may show resistance to using mint-flavored dental floss. Try offering them different flavors of dental floss to find the one most acceptable to your child. If that doesn’t work, using an oral irrigator may help.
Establish routines
It is important to encourage the habit of brushing the teeth after each meal and placing hygiene items in a fixed and accessible place, so the child can find them easily.
Use timers
Children with autism often have difficulty brushing for the dentist-recommended two-minute period, as they may want to finish it quickly. Provide some sort of timer, such as an hourglass, kitchen timer, or even a timer built into your toothbrush to help them maintain the proper duration of brushing.
Remember that each child is unique, so it is important to tailor these tips to the individual needs of each autistic patient. It’s important to start early.
If you want to learn more, we have a guide about when to start brushing a baby’s teeth.
Conclusion
We can all agree dental treatment in children with autism can be difficult. Fortunately, there are professionals trained to guide oral care for these patients.
Frequently Asked Questions
How do kids with autism go to the dentist?
Traditional treatment. With patience and empathy, numerous children and adults with autism can manage a standard dental appointment without the need for restraints or sedation. Based on my experience, this approach includes guiding the patient through each procedure and employing positive reinforcement to achieve the goals of the visit.
How does autism affect dental care?
Behavioral challenges such as hyperactivity and easy frustration can make oral health care more difficult for patients with autism. The invasive aspects of dental care can provoke aggressive and self-harming behaviors like temper tantrums or head banging.
What are the dental problems with children with autism?
Excessive grinding and clenching of the teeth, both during the day and at night, can lead to gradual wear of the tooth surface, pain, tooth loss, and jaw problems. This grinding and wear can be triggered by stress, improper biting positions, medication side effects, epilepsy, seizures, developmental tooth defects, and missing teeth.
Is general anesthesia safe for an autistic child?
Deciding whether to sedate your autistic child for dental and diagnostic procedures can be stressful because anesthesia can worsen underlying health issues common in autism. However, it’s crucial to understand that with the right precautions, children with autism can be sedated safely.
Should I tell my dentist I'm autistic?
While it’s not mandatory for autistic individuals to disclose their diagnosis to their dentist, doing so can be beneficial. By sharing this information, the dentist can make specific adjustments before and after treatment to improve the experience. These adjustments should be tailored to meet the patient’s unique needs and level of understanding.
Share:
References
1. A guide to dental care for children with autism. (2022). Byte.com.
2. Caregiver’s Guide, A. (2012). Dental care every day. Nih.gov. https://www.nidcr.nih.gov/sites/default/files/2017-09/dental-care-every-day-caregiver.pdf
3. Fred (c), I. C. D., & MEd, N. B. M. (Jun 29, 2021). Making visits to the dentist easier for people with autism spectrum disorder. Harvard Health. https://www.health.harvard.edu/blog/making-visits-to-the-dentist-easier-for-people-with-autism-spectrum-disorder-202106292513
4. Lichty, J. (Apr 18, 2019).A dental visit guide for children with autism & sensory issues – children’s dental health. Children’s Dental Health. https://childrensdentalhealth.com/dental-visit-guide-for-children-with-autism-sensory-issues/
5. Stein, L. I., Polido, J. C., Mailloux, Z., Coleman, G. G., & Cermak, S. A. (2011). Oral care and sensory sensitivities in children with autism spectrum disorders. Special care in dentistry: official publication of the American Association of Hospital Dentists, the Academy of Dentistry for the Handicapped, and the American Society for Geriatric Dentistry, 31(3), 102–110. https://onlinelibrary.wiley.com/doi/10.1111/j.1754-4505.2011.00187.x
6. Chandrashekhar, S., & S Bommangoudar, J. (2018). Management of Autistic Patients in Dental Office: A Clinical Update. International Journal of clinical pediatric dentistry, 11(3), 219–227. https://doi.org/10.5005/jp-journals-10005-1515
-
Nayibe Cubillos M. [Author]
Pharmaceutical Chemestry |Pharmaceutical Process Management | Pharmaceutical Care | Pharmaceutical Services Audit | Pharmaceutical Services Process Consulting | Content Project Manager | SEO Knowledge | Content Writer | Leadership | Scrum Master
View all posts
A healthcare writer with a solid background in pharmaceutical chemistry and a thorough understanding of Colombian regulatory processes and comprehensive sector management, she has significant experience coordinating and leading multidisciplina...Recent Posts