Last Updated on: 10th December 2025, 06:33 am
The Side Effects of Antiepileptic Drugs on Oral Health?
Epilepsy is a chronic, non-communicable brain disease in which seizures are generated. According to the WHO, this is the most common neurological disorder. About 50 million people in the world suffer from it.
Epilepsy can lead to clenching the jaws and grinding the teeth, among other effects. We have a comprehensive guide about bruxism and epilepsy that can help you understand the connection between the two.
With proper treatment, most people can live without seizures. However, to achieve this goal, some medications are prescribed that, while fulfilling their basic function can engender side effects on oral health.
What are Antiepileptic Drugs?
Antiepileptics are drugs widely used in the treatment of seizure disorders (such as epilepsy), neuropathic pain, and psychiatric disorders. They act on the central nervous system, so their chronic consumption can have multiple side effects, including drowsiness, dizziness, and loss of balance. In some cases, they can generate side effects on the gastrointestinal system and the oral cavity. This is a problem because these treatments are usually lifelong or long-lasting, implying the need to deal medically with the adverse effects of the medication.
What are the Most Used Antiepileptic Drugs?
The most frequently prescribed antiepileptic drugs are:
• Carbamazepine
• Phenytoin
• Lamotrigine
• Sodium valproate
• Gabapentin
• Clonazepam
• Lorazepam
• Diazepam
• Phenobarbital
Oral Complications of Antiepileptic Drugs
As mentioned, antiepileptic drugs are effective in treating various diseases, but prolonged use can have side effects on the patient’s oral health.
1. Gingival hypertrophy or enlargement
This is one of the most common oral complications associated with the long-term use of antiepileptic drugs. It manifests as an increase in the size of the gums, which can affect both aesthetics and oral function.
Although it is usually painless, patients may experience difficulty speaking, chewing, and swallowing, as well as gum bleeding and changes in tooth positions. An increase in the size of the gums also generates retention of food debris and bacteria on the surface of the teeth. Drugs linked to this condition include phenytoin, carbamazepine, and sodium valproate. To understand moresigns and symptoms of gum disease, click here.
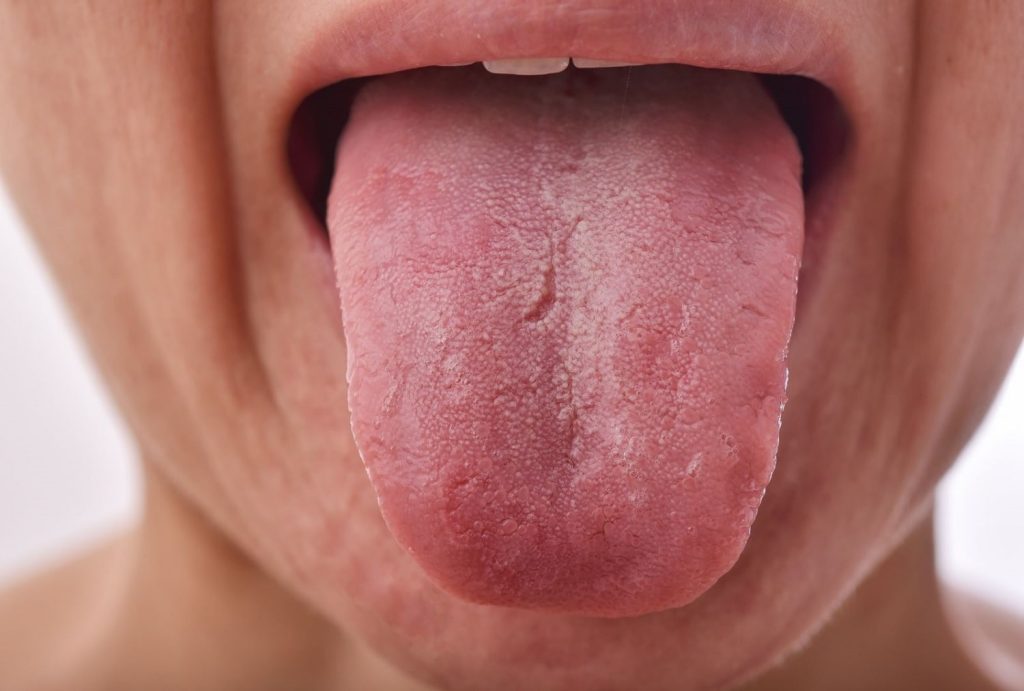
2. Xerostomia
Xerostomia, hyposalivation, or dry mouth, is another common oral complication associated with the use of antiepileptic drugs. Patients may experience decreased saliva production, which can cause dental caries, periodontal disease, and a predisposition to lacerations of the oral mucosa. Xerostomia can also cause problems swallowing food and taste disturbances.
3. Hematopoietic disorders
The hematopoietic system is responsible for producing blood cells. Some antiepileptic drugs have been shown to alter the production of these cells, affecting coagulation and causing lesions in the gums and mucosa.
Can Antiepileptic Drugs cause Cavities?
Antiepileptic drugs can cause caries indirectly by decreasing salivary flow. Saliva is essential to protect teeth from caries since it cleans surfaces, maintains an optimal pH, and helps to constantly remineralize dental tissue. Therefore, patients with xerostomia or decreased salivation are more prone to developing caries.
Oral Health Considerations in Patients with Epilepsy
If you suffer from epilepsy, the following tips may be helpful:
• Schedule your appointments at a time when seizures are unlikely.
• Tell your dentist about the type and frequency of seizures.
• Do not stop anticonvulsant medications if the treating physician has not indicated it.
• Tell your dentist what triggers your seizures so he can take preventive measures, such as wearing dark glasses or eye masks with stress management techniques.
• Although it is not commonly required, the use of conscious sedation is an option for patients for whom dental care generates a high level of anxiety; You can request it if you need it.
• Make sure that the health professional adapts the consultation to your needs. If this does not happen, it is advisable to look for another service provider.
• If you require the use of prostheses, if possible they should not be removable to avoid choking during seizures.
• If the use of removable dental prostheses is unavoidable, opt for metal prostheses to avoid the risk of fracture.
• Attend dental check-ups every six months.
If you require more information on dental health in patients with epilepsy, you can consult our post on bruxism and epilepsy.
Conclusion
• Antiepileptic drugs are used to treat various diseases in addition to seizure disorders.
• Although antiepileptics are effective, they can induce side effects or complications in the oral cavity.
• It is important that both the patient and the dentist are aware of these complications to prevent and treat them effectively.
Frequently Asked Questions
Do antiepileptic drugs affect oral health in patients with epilepsy?
Yes, antiepileptic drugs can affect oral health in patients with epilepsy. These medications can cause several oral complications, including gingival hypertrophy (gum enlargement), xerostomia (dry mouth), and hematopoietic disorders, which can lead to increased risk of gum disease, cavities, and other oral health issues.
What are the adverse effects of antiepileptic drugs?
The adverse effects of antiepileptic drugs on oral health include:
- Gingival hypertrophy: Enlargement of the gums, which can affect aesthetics, speech, chewing, and increase the risk of gum disease.
- Xerostomia: Reduced saliva production, leading to dry mouth, increased risk of cavities, periodontal disease, and oral mucosa lacerations.
- Hematopoietic disorders: Affecting blood cell production, which can impair blood clotting and cause lesions in the gums and oral mucosa.
Can antiepileptic drugs cause oro-facial trauma?
Yes, antiepileptic drugs can indirectly contribute to oro-facial trauma. Patients with epilepsy are at risk of seizures, which can result in falls and injuries to the face and mouth. Additionally, side effects like drowsiness and loss of balance from these medications can increase the likelihood of accidents leading to facial trauma.
Dental management of epilepsy
Effective dental management of epilepsy involves:
- Informing the dentist about the epilepsy diagnosis and medications being taken.
- Scheduling dental appointments at times when seizures are less likely to occur.
- Ensuring the dentist is aware of seizure triggers and taking preventive measures, such as using stress management techniques and dark glasses.
- Avoiding cessation of anticonvulsant medications without the treating physician’s consent.
- Considering conscious sedation for patients with high anxiety levels during dental care.
- Opting for fixed dental prostheses when possible to prevent choking hazards during seizures.
Dental health tips for patients taking antiepileptic drugs
Patients taking antiepileptic drugs should follow these tips for maintaining good oral health:
- Inform the dentist about all medications being taken to avoid interactions and enhanced adverse effects.
- Visit the dentist every six months for check-ups, preventive cleanings, and early detection of cavities and gum disease.
- Maintain excellent oral hygiene by brushing teeth three times a day with fluoride toothpaste and flossing daily.
- If experiencing significant gum enlargement, consult a dental professional; surgical removal of excess gum tissue may be necessary.
- Manage xerostomia by drinking plenty of water, chewing sugarless gum, avoiding acidic or sugary foods, and using alcohol-free mouthwash.
- Limit caffeine intake and ask the dentist about over-the-counter salivary substitutes if needed.
Share:
References
1. Aragon, C. E., & Burneo, J. G. (2007). Understanding the patient with epilepsy and seizures in the dental practice. Journal (Canadian Dental Association), 73(1), 71–76.
2. Cornacchio, A. L. P., Burneo, J. G., & Aragon, C. E. (2011). The effects of antiepileptic drugs on oral health. Journal (Canadian Dental Association), 77, b140. https://jcda.ca/article/b140
3. Dry mouth. (Feb 1, 2011). Mayoclinic.org. https://www.mayoclinic.org/diseases-conditions/dry-mouth/diagnosis-treatment/drc-20356052
4. Epilepsy. (s/f). Who.int.https://www.who.int/news-room/fact-sheets/detail/epilepsy
5. Gallo, C., Bonvento, G., Zagotto, G., & Mucignat-Caretta, C. (2021). Gingival overgrowth induced by anticonvulsant drugs: A cross-sectional study on epileptic patients. Journal of Periodontal Research, 56(2), 363–369. https://onlinelibrary.wiley.com/doi/10.1111/jre.12828
6. Joshi, S. R., Pendyala, G. S., Saraf, V., Choudhari, S., & Mopagar, V. (2013). A comprehensive oral and dental management of an epileptic and intellectually deteriorated adolescent. Dental research journal, 10(4), 562–567.
- Nayibe Cubillos M. [Author]
Pharmaceutical Chemestry |Pharmaceutical Process Management | Pharmaceutical Care | Pharmaceutical Services Audit | Pharmaceutical Services Process Consulting | Content Project Manager | SEO Knowledge | Content Writer | Leadership | Scrum Master
View all posts
A healthcare writer with a solid background in pharmaceutical chemistry and a thorough understanding of Colombian regulatory processes and comprehensive sector management, she has significant experience coordinating and leading multidisciplina...