Last Updated on: 19th September 2025, 12:31 pm
An oral mucocele might seem like a small thing, but it can quickly become one of those little problems that get in the way of your daily life. It often appears as a soft bump inside your mouth, usually on your lip or under the tongue; while it’s not dangerous, it can be pretty annoying. It might make it uncomfortable to talk, eat, or even smile.
Thankfully, mucoceles are usually easy to identify and, in many cases, don’t require complicated treatment. In this post, we’ll guide you through what a mucocele is, why it appears, how to recognize one, and the treatment options available to help you get back to feeling comfortable in no time.
What is an oral mucocele?

An oral mucocele, or mucous cyst, is a small fluid-filled lump that forms inside the mouth. It develops when the duct of a salivary gland becomes blocked or damaged, causing a buildup of mucus in the surrounding tissues. The result is a soft, rounded swelling, often light-colored, bluish, or pinkish.
These cysts are usually painless and harmless and, in many cases, disappear on their own without treatment. However, depending on their size and location, they can be bothersome, especially if they interfere with eating, talking, or brushing the teeth.
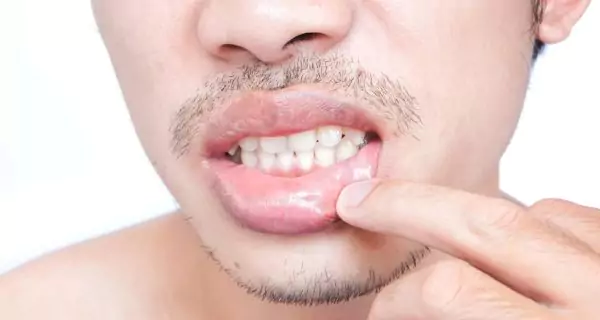
Where do mucoceles appear?
Mucoceles can develop anywhere in the mouth where minor salivary glands are present. They’re most commonly found on the:
- inner surface of the lower lip (by far the most frequent location)
- upper lip
- cheeks (inside)
- underside or tip of the tongue
- floor of the mouth (when located here, it’s known as a ranula)
They can range in size from a few millimeters to as large as 3 centimeters and may appear either close to the surface or deeper in the tissue.
Why is it important to treat an oral mucocele?
While oral mucoceles are usually harmless and non-cancerous that doesn’t mean they should be ignored, especially if they don’t go away on their own.
If left untreated, a mucocele can lead to a range of discomforts and complications, such as:
- pain or irritation, especially as the cyst grows
- difficulty speaking, if it interferes with tongue or lip movement
- problems with chewing or eating
- inflammation or damage to the surrounding tissues
- infection, which may occur if the area becomes injured or irritated repeatedly
Common causes of oral mucoceles
Most mucoceles are caused by trauma to a salivary gland duct, which either blocks the duct or causes it to rupture. This allows mucus to leak into the surrounding tissue, forming a lump.
Common triggers Include:
- biting the lip or cheek, often during eating, talking, or while sleeping
- repetitive habits, like lip or cheek biting, or chewing on pens or nails
- friction or irritation from braces, piercings, or poorly fitted dentures
- accidental injuries, such as facial trauma or burns from hot foods
- blockages caused by thick saliva, debris, or inflammation
- medical conditions, like Sjögren’s syndrome or chronic dry mouth, that affect saliva production
In some cases, mucoceles can appear spontaneously, without a clear trigger, possibly due to subtle, unnoticed damage to the gland.
Who is most likely to get a mucocele?

Anyone can get a mucocele, but they are more frequently seen in:
- Children and teenagers, due to more frequent bumps, bites, and the use of orthodontic appliances.
- Young adults, particularly those with piercings or oral habits like nail-biting.
- Older adults, especially in cases where dry mouth or blocked ducts are common.
Understanding the causes and risk factors can help prevent mucoceles or reduce the chance of them coming back.
Types of mucoceles
Mucoceles are generally classified into two main types based on how they form:
1. Extravasation mucocele (most common)
- Cause: rupture of a salivary duct that allows mucus to spill into surrounding tissues
- Typical in: children and adolescents
- Triggers: biting, friction from braces, piercings, or trauma
- Location: most often appears on the inner lower lip
This is the most frequent type, accounting for 70–80% of cases, often linked to everyday irritation or injury.
2. Retention mucocele (less common)
- Cause: blockage inside the salivary duct, leading to trapped saliva
- Typical in: adults over 30 or 40 years old
- Triggers: thick saliva, small particles, or impurities that clog the duct
- Location: can occur anywhere, often deeper in the tissue
Though less common, retention mucoceles may need thorough management if they don’t resolve on their own.
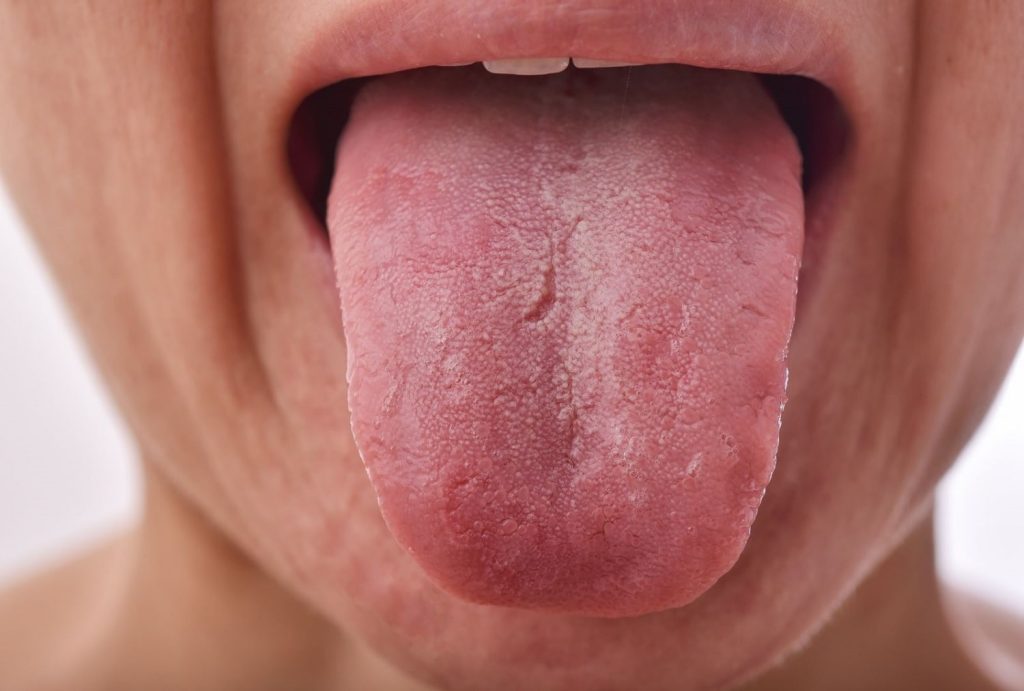
Symptoms of an oral mucocele

An oral mucocele typically appears as a soft, round bump inside the mouth, often on the lower lip, cheeks, or under the tongue. It’s usually painless but may cause discomfort depending on its location. Key symptoms include:
- bluish or translucent swelling
- no pain, but possible discomfort when eating or speaking
- a sense of pressure or fullness in the area
- fluctuating size, it may shrink, burst, and reappear
- occasional redness or irritation, especially if bitten
Even though it’s usually not serious, you should see a dentist if the bump doesn’t go away or starts to change.
When should you see a dentist for a mucocele?
Most mucoceles are harmless and go away on their own, but that doesn’t mean you should ignore them completely. It’s important to keep an eye on the size and symptoms of the bump. If anything changes or worsens, it may be time to get it checked.
You should consider seeing a dentist or oral specialist if the mucocele:
- grows in size
- lasts longer than a few weeks without improvement
- becomes painful or uncomfortable
- interferes with eating, speaking, or daily activities
- keeps coming back in the same area
- shows signs of irritation or infection
Getting an early diagnosis and proper treatment will help prevent complications, such as infection or the need for more invasive procedures later on. A professional will confirm whether it’s a mucocele and recommend the best course of action based on your specific case.
Treatment options for oral mucoceles

While some mucoceles may resolve on their own, others may require medical intervention. Treatment options vary depending on the size, location, and persistence of the mucocele. Below are the most common treatments for oral mucoceles.
Observation and home care
For small mucoceles that aren’t causing discomfort, a “watch and wait” approach is often enough. Simple at-home steps include:
- warm saltwater rinses several times a day to reduce inflammation and promote healing
- avoiding spicy, hot, or acidic foods that might irritate the area
- staying hydrated to keep saliva flowing normally
- maintaining good oral hygiene to prevent secondary infections
- not biting or touching the bump to avoid worsening the irritation
These remedies don’t cure the cyst but may support the healing process. Never try to pop or drain a mucocele yourself, as this can lead to infection or further tissue damage.
Medical treatments (non-surgical)

When home care isn’t enough or the cyst is causing mild discomfort, non-invasive treatments may be recommended. Common options include:
- topical corticosteroids to reduce inflammation
- anti-inflammatory medications (prescribed or over-the-counter) for pain relief
- needle aspiration, using a fine needle to release trapped fluid (offers temporary relief, but often recurs)
Minimally invasive procedures
For stubborn or recurring mucoceles, minimally invasive techniques may be more effective and less disruptive than traditional surgery.
- Laser therapy: a quick, low-discomfort method that uses a focused beam of light to remove the cyst. It reduces bleeding, promotes faster healing, and lowers the risk of recurrence.
- Cryotherapy: freezing the cyst with extreme cold, typically used for smaller mucoceles.
- Marsupialization: involves opening the mucocele and suturing the edges to create a small permanent opening, allowing continuous drainage and preventing buildup.
These methods are usually performed under local anesthesia and offer a quicker recovery than full surgery.
Surgical options
For larger, chronic, or recurrent mucoceles, surgery may be the best solution. The procedure is safe, quick, and often done under local anesthesia.
Surgical techniques include:
- Cystectomy: full removal of the mucocele along with its sac or capsule, typically used when the lesion is well-contained.
- Cystostomy: creating an opening to allow fluid drainage, especially when the cyst is close to important structures.
- Complete excision: removing the cyst and the affected salivary gland to prevent future recurrence. This is sometimes necessary if the same mucocele keeps returning.
Recovery from surgical or laser treatment is usually fast. Most people recover fully within 1–2 weeks, and recurrence is low with proper care. Your dentist could recommend you:
- anti-inflammatory medications
- chlorhexidine rinses to keep the area clean
- a soft diet and avoiding hot foods or drinks for a few days
Preventing mucoceles: what you can do

While mucoceles aren’t always preventable, there are simple steps you can take to reduce your risk:
- Avoid biting or sucking on your lips and cheeks, especially if it’s a habit.
- If you wear braces or dentures, use orthodontic wax or ask your dentist about adjustments to prevent friction and irritation.
- Maintain good oral hygiene to lower the risk of infection, especially after treatment.
- Stay hydrated and avoid overly spicy or acidic foods that can irritate the soft tissues.
- Use a mouth guard if you practice contact sports to avoid bumps in the mouth.
- Schedule regular dental check-ups so your dentist can monitor your oral health and catch any early signs of issues like mucoceles.
With the right care and attention, mucoceles can be managed easily and in many cases, prevented altogether.
Conclusion
While generally benign, oral mucoceles can cause discomfort and affect your oral health. Understanding the causes, symptoms, and treatment options will help you manage this condition effectively.
While some mucoceles may resolve on their own, others may require intervention through drainage, surgical removal, or laser therapy. If you suspect you have a mucocele, or if it is causing discomfort or interference with daily activities, it’s best to consult with a dental professional to determine the most appropriate treatment.
Taking care of your mouth isn’t just about your teeth; it’s about your overall comfort and confidence.
Frequently Asked Questions
Can I pop a mucocele at home?
Is a mucocele contagious?
How long does it take for a mucocele to heal after removal?
What causes a mucocele to keep coming back?
Can I eat normally if I have a mucocele?
Share
References
1. Cleveland Clinic Collaborators. (2022). Oral Mucocele. https://my.clevelandclinic.org/health/diseases/23406-oral-mucocele
2. More, C. B., Bhavsar, K., Varma, S., & Tailor, M. (2014). Oral mucocele: A clinical and histopathological study. Journal of oral and maxillofacial pathology: JOMFP, 18(Suppl 1), S72–S77. https://journals.lww.com/jpat/fulltext/2014/18001/oral_mucocele__a_clinical_and_histopathological.15.aspx
3. Ngan, V. (2005). Mucocele of the lip. DermNet. https://dermnetnz.org/topics/mucocoele-of-the-lip
4. Rao, P. K., Hegde, D., Shetty, S. R., Chatra, L., & Shenai, P. (2012). Oral mucocele – Diagnosis and management. Journal of Dentistry, Medicine and Medical Sciences Vol. 2(2) pp. 26-30, November 2012. https://www.interesjournals.org/articles/oral-mucocele–diagnosis-and-management.pdf
5. Stuart, A. (2025, 22 January). Oral Mucous Cyst. WebMD. https://www.webmd.com/oral-health/mucocele-causes-symptoms-and-treatment
- Dr. Yeidy Carolina Mesa [Author]
DDS Yeidy Carolina Mesa Passionate Dentist | Advocate for Accessible Oral Health Education Graduating from Universidad CES in 2022, I am a dedicated general dentist with a lifelong passion for helping others and making a meaningful impact in the world. My journey into dentistry began at the age of 7, inspired by my own experience with braces and overcoming a fear of the dentist. This personal journey shaped my mission to help patients conquer their own dental anxieties and embrace a healthier,...
View all posts
- Nayibe Cubillos M. [Medical Reviewer]
Pharmaceutical Chemestry |Pharmaceutical Process Management | Pharmaceutical Care | Pharmaceutical Services Audit | Pharmaceutical Services Process Consulting | Content Project Manager | SEO Knowledge | Content Writer | Leadership | Scrum Master
View all posts
A healthcare writer with a solid background in pharmaceutical chemistry and a thorough understanding of Colombian regulatory processes and comprehensive sector management, she has significant experience coordinating and leading multidisciplina...Recent Posts