Last Updated on: 2nd January 2026, 10:41 am
What is jaw bone cavitation?
The first thing that must be taken into account regarding this condition is to clarify the terms and their differences. It is very common to confuse the term cavity with cavitation. In dentistry, a dental cavity refers to a hole in the dental surface, generally appearing when there is a cavity. Cavitation refers to a hole in the surface of the bone, but the term can be used both in medicine and dentistry, since it can occur in any bone.
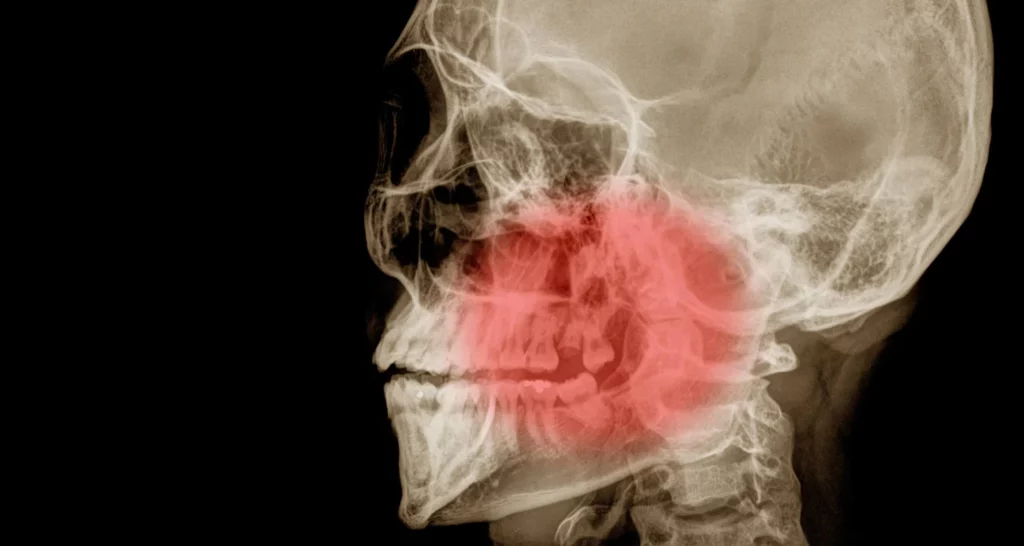
Jaw bone cavitation is also known as cavitational osteonecrosis or ischemic osteonecrosis. It is a serious pathology that occurs after having suffered an infectious process, inflammation or necrosis within the jaw. The typical treatment is surgery.
What can cause jaw bone cavitation?
Jaw bone cavitation is an injury that can compromise both the mandible and maxilla. It has no apparent cause and can occur spontaneously or after a dental extraction. It can also be caused by trauma (strong blows) or pharmacological treatments with a high dose of bisphosphonates, although it has not been shown that their use is directly related to the development of cavitation. However, it is recommended to carry out other dental treatments before starting with bisphosphonates, chemo or radiotherapy.
What are the symptoms of osteonecrosis of the jaw or jaw bone cavitation?
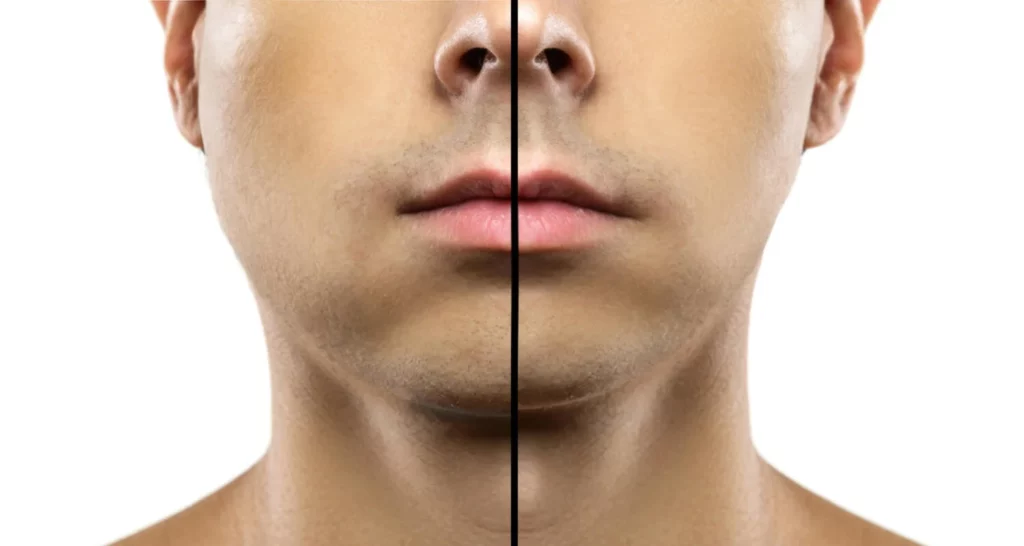
Jaw cavitation may not have manifest symptoms for a long period of time. When the cavitation is in an advanced stage, there is usually pain, purulent discharge, and the exposed jaw bone can be observed. It can also occur in the maxilla, although less frequently. The teeth and gums can be compromised, and fistulas can also develop inside or outside the mouth.
How can you recognize the symptoms of jaw bone cavitation?
As a disease that occurs without symptoms, it is important to recognize changes in the tissues of the mouth, especially after a dental treatment. Severe pain, accompanied by purulent discharge, bad breath. There may be warning signs and a specialist should be consulted immediately. The bacteria and toxic substances accumulated in the affected area can reach the circulation through the nervous tissue, affecting other cells and organs of the body, causing episodes of:
● Generalized inflammation
● Chronic fatigue
● General discomfort
Is there treatment for jaw bone cavitation?
The diagnosis of the disease should be made after a clinical evaluation. the dentist can request an X-ray or tomography to confirm the diagnosis and suggest a treatment plan that may include:
● Limited debridement, antibiotics, and mouthwashes such as chlorhexidine.
● Surgical Recession: should be the last option to consider as recession can make the condition worse.
Can jaw bone cavitation be prevented?
Jaw cavitation is a rare pathology, and as such, it does not have a specific cause. However, it is associated with the ingestion of certain medications such as bisphosphonates, medications for osteoporosis, or bone exposure for at least 8 weeks after a dental extraction. It is important to inform the dentist about the consumption of medications or chemo or radiotherapy treatments before performing any treatment, especially dental extractions since these factors increase the probability of developing bone necrosis after dental treatments.
These factors significantly elevate the risk of developing bone necrosis after dental procedures. Additionally, individuals who have not experienced the closure of a wisdom tooth hole should also provide this information to their dentist.
Conclusion
It is very important to inform the dentist and oral surgeon that you are undergoing treatment with medications such as bisphosphonates, treatment for osteoporosis, or if you have been or are undergoing chemotherapy or radiotherapy treatment since these factors promote the development of mandibular bone cavitation. It is advisable to perform oral surgeries or dental treatments before starting a pharmacological or oncological treatment to avoid this complication.
However, it does not mean that dental treatment cannot be done during atreatment. It is not highly recommended; but if you can do it, take into account that dental treatments must be done by specialists such as the oral or maxillofacial surgeon – always in support of the treating physician. In addition, having good oral hygiene habits, a balanced diet, and a healthy lifestyle all help to avoid complications that can put your health at risk.
Frequently Asked Questions
What is jaw bone cavitation?
Jaw bone cavitation, also known as cavitational osteonecrosis or ischemic osteonecrosis, is a serious condition where a hole forms in the surface of the jawbone. This occurs due to an infectious process, inflammation, or necrosis within the jaw. It should not be confused with a dental cavity, which refers to a hole in the tooth surface.
What can cause jaw bone cavitation?
Jaw bone cavitation can occur spontaneously or following a dental extraction. Other potential causes include trauma (such as strong blows) and high-dose bisphosphonate treatments. Although the direct relationship between bisphosphonates and cavitation has not been conclusively proven, it is advisable to complete any necessary dental treatments before starting bisphosphonate, chemotherapy, or radiotherapy treatments.
What are the symptoms of jaw bone cavitation?
Jaw bone cavitation may initially present without symptoms. As it progresses, symptoms can include severe pain, purulent discharge, and visible exposure of the jawbone. Other symptoms might include compromised teeth and gums, and the development of fistulas inside or outside the mouth.
How is jaw bone cavitation diagnosed and treated?
A dentist will diagnose jaw bone cavitation through clinical evaluation and may request an X-ray or tomography for confirmation. Treatment options may include limited debridement, antibiotics, and mouthwashes such as chlorhexidine. Surgical recession is considered a last resort as it can sometimes worsen the condition.
Can jaw bone cavitation be prevented?
While jaw cavitation is a rare condition without a specific cause, preventive measures include informing your dentist about any medications like bisphosphonates or treatments such as chemotherapy or radiotherapy before undergoing dental procedures.
Good oral hygiene, a balanced diet, and a healthy lifestyle can also help mitigate risks. Always consult with specialists like oral or maxillofacial surgeons, especially if undergoing concurrent pharmacological or oncological treatments.
Share:
References
1. A. Khan, A. M. (October 22, 2015). Springer. Obtained from Osteonecrosis of the jaw (ONJ): diagnosis and management in 2015: https://rd.springer.com/article/10.1007/s00198-015-3335-3
2. Bülent Atilla, S. B. (28 de january de 2020). Efort open reviews. Obtenido de Joint-preserving procedures for osteonecrosis of the femoral head: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6986391/
3. Goodman, S.B. (September 01, 2021). MSD Manual. Retrieved from Osteonecrosis: https://www.msdmanuals.com/es-co/professional/trastornos-de-los-tejidos-musculoesquel%C3%A9tico-y-conectivo/osteonecrosis/osteonecrosis-on
4. John W Hellstein, R. A. (01 de Noviembre de 2011). Journal of the American Dental Association. Obtenido de Managing the care of patients receiving antiresorptive therapy for prevention and treatment of osteoporosis: executive summary of recommendations from the American Dental Association Council on Scientific Affairs: https://pubmed.ncbi.nlm.nih.gov/22041409/
5. John W Hellstein, R. A. (01 de Noviembre de 2011). Journal of the American Dental Association. Obtenido de Managing the care of patients receiving antiresorptive therapy for prevention and treatment of osteoporosis: executive summary of recommendations from the American Dental Association Council on Scientific Affairs: https://pubmed.ncbi.nlm.nih.gov/22041409/
6. Crit Boontanapibul, J. T. (May 05, 2020). National Library of Medicine. Obtained from Diagnosis of Osteonecrosis of the Femoral Head: Too Little, Too Late, and Independent of Etiology: https://pubmed.ncbi.nlm.nih.gov/32456965/
7. Lechner J, S.T. (March 21, 2021). dovepress. Retrieved from RANTES/CCL5 Expressed Mandibular Cavitation: Case Studies Linking Silent Inflammation in the Jaw Bone to Breast Cancer Epistemology: https://www.dovepress.com/jawbone-cavitation-expressed-rantesccl5-case-studies-linking-silent-in-peer-reviewed-fulltext-article-BCTT
8. Marincola, M. (January 1, 2014). Implants. Retrieved from Jawbone cavitation and its involvement in implant dentistry.
-
DDS Juliana Garzon [Author]
Dr. Juliana Garzón Ariza Endodontics Specialist | Passionate Advocate for Oral Health Transformation Graduating from the esteemed Universidad Nacional de Colombia in 2021, I am a dentist and a final-year resident specializing in Endodontics. My professional mission is to transform oral health through prevention, highly specialized treatments, and patient education. With a strong focus on dental research, I am driven to innovate solutions in critical areas such as dental pain, infections, dent...
View all posts
-
Nayibe Cubillos M. [Medical Reviewer]
Pharmaceutical Chemestry |Pharmaceutical Process Management | Pharmaceutical Care | Pharmaceutical Services Audit | Pharmaceutical Services Process Consulting | Content Project Manager | SEO Knowledge | Content Writer | Leadership | Scrum Master
View all posts
A healthcare writer with a solid background in pharmaceutical chemistry and a thorough understanding of Colombian regulatory processes and comprehensive sector management, she has significant experience coordinating and leading multidisciplina...