Last Updated on: 19th September 2025, 12:30 pm
Yes, Antiphospholipid Antibody Syndrome (APS) can affect your oral health by increasing bleeding during dental procedures, causing painful mouth ulcers while raising the risk of gum disease, especially in patients taking blood thinners.
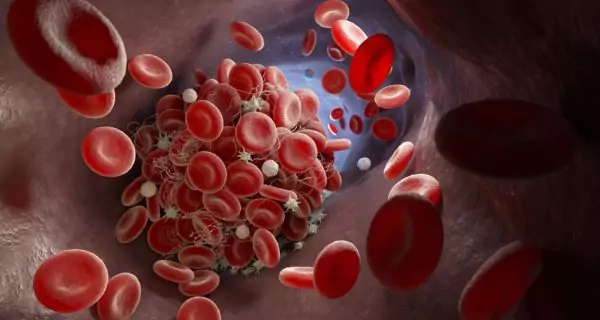
Have you ever heard about Antiphospholipid Antibody Syndrome or know someone who has it? This autoimmune condition affects the blood’s ability to clot properly. While most people know about its risks for stroke, thrombosis, or pregnancy complications, fewer realize that it can also affect the mouth.
In this article, we’ll explain what APS is, its impact on your oral health, and the steps you can take to protect your smile and overall well-being.
What is Antiphospholipid Antibody Syndrome (APS)?
Antiphospholipid Antibody Syndrome (APS) is an autoimmune disorder in which the immune system mistakenly produces antibodies that cause the blood to clot more easily than it should.
These abnormal clots can form in both arteries and veins, leading to serious health problems like:
- deep vein thrombosis
- strokes or heart attacks
- miscarriages and pregnancy complications
APS affects 3 to 5 times more women than men, and most people are diagnosed between the ages of 20 and 50. It can occur on its own or with other autoimmune diseases like lupus.
While it’s typically seen as a blood-related condition, its impact doesn’t stop there; it can also lead to important changes in your mouth. That’s exactly what we’ll explore next.
What oral problems are common in people with APS?
To understand the connection between Antiphospholipid Antibody Syndrome (APS) and oral health, it helps to know how this condition affects the mouth.
The main reason lies in the treatment. Most people with APS are prescribed blood-thinning medications to reduce the risk of clots. These include:
- Warfarin
- Heparin
- Enoxaparin
While these medications are essential for preventing serious complications, they can create challenges when it comes to oral care. Below, we’ll explain what these risks are and what you should watch out for.
Why do people with APS bleed more during dental treatments?
Blood thinners reduce the blood’s ability to clot. Imagine your blood becoming thinner or more watery. Even a small cut or injury inside the mouth can lead to prolonged or excessive bleeding.
Procedures like professional cleanings, extractions, or surgeries require special care to avoid complications. Dentists must be aware of your condition to plan properly and take the necessary extra steps to manage bleeding safely.
Can APS cause mouth sores or ulcers?
Yes, some people with APS develop painful ulcers or sores inside the mouth on the tongue, cheeks, or gums. These can be related to the body’s autoimmune response or even to medication side effects.
While not everyone with Antiphospholipid Antibody Syndrome will have them, those who do may find eating, speaking, or brushing their teeth uncomfortable or painful.
Are swollen or bleeding gums more common with APS?
Definitely. People with APS, especially those taking anticoagulants, may notice that their gums are more sensitive and swollen, or bleed easily, even with gentle brushing.
In many cases, this is a sign of gingivitis, the early stage of gum disease. It’s reversible if treated promptly; but if it’s ignored, it can progress and cause more serious problems.
Does APS increase the risk of periodontitis?
Yes, if gingivitis is not addressed, it can lead to periodontitis, a more serious infection that damages the tissues and bone that support the teeth.
For people with APS, this risk is even higher. Their gums are often more vulnerable and their healing response may be slower due to medication.
What should your dentist know if you have APS?
If you have Antiphospholipid Antibody Syndrome (APS), visiting the dentist requires more than just booking an appointment.
From the very first visit, it’s important to let your dentist know about your diagnosis. They can apply safe, effective, and adapted care for your specific needs.
While good oral hygiene and regular check-ups are essential to prevent problems, dental professionals must also take extra steps when working with APS patients.
Should the dentist review my medical history?
Yes, before any dental procedure, your dentist should review your full medical background, including:
- Whether your APS is primary or linked to another disease, like lupus
- The medications you’re currently taking, especially blood thinners
- Your latest blood test results, such as your INR level if you’re on warfarin
This information helps the dentist understand your risk level in order to make safe decisions about your treatment.
Does the dentist need to talk to my doctor?
Yes, if you need a surgical or invasive procedure, like a tooth extraction, your dentist should contact your primary care doctor or hematologist. These professionals will decide:
- if your medication should be adjusted or paused
- whether additional precautions are needed
- if the dental treatment should be delayed or done in a controlled setting
Never stop taking your anticoagulants without medical approval.
Can dental procedures be made safer?
Yes, whenever possible, your dentist may recommend non-invasive treatments to avoid unnecessary risks. If surgery is necessary, there are ways to minimize bleeding and support healing, such as:
- using local hemostatic agents (products that help stop bleeding)
- applying precise sutures to close wounds properly
- giving you detailed aftercare instructions to reduce complications
How can you take care of your mouth if you have APS?
When you live with Antiphospholipid Antibody Syndrome, prevention is your best tool.
Taking care of your mouth every day helps you avoid complications like bleeding, infections, or gum disease, which can be harder to manage due to your condition and medications.
Here are some easy and effective ways to protect your oral health at home:
How should you brush your teeth?
Brush gently, but thoroughly. Use a soft-bristled toothbrush and clean your teeth at least twice a day, using small, circular motions.
You don’t need to press hard; being gentle is safer for your gums, especially if you’re taking blood thinners.
Can you floss if you take blood thinners?
Yes, but do it carefully. Flossing is important to remove plaque and food between the teeth, but it must be done gently to avoid irritating the gums.
If floss feels too harsh or difficult to use, try alternatives like:
- interdental brushes: perfect for wider gaps or sensitive areas
- oral irrigators (water flossers): they clean between teeth using a gentle stream of water, and feel like a soft massage for your gums
What can you do about dry mouth?
Many people with APS experience dry mouth, often due to prescribed medications. A dry mouth can increase your risk of cavities, bad breath, and discomfort while speaking or eating.
To keep your mouth hydrated:
- Drink water regularly throughout the day.
- Use sugar-free gum or lozenges to stimulate saliva.
- Try saliva substitutes or hydrating oral gels.
- Choose an alcohol-free mouthwash to avoid extra dryness.
If a dry mouth becomes persistent or uncomfortable, talk to your dentist. They will recommend the right products for your case.
What kind of toothpaste should you use?
Choose a fluoride toothpaste to strengthen your enamel and protect your teeth. If your gums are sensitive or prone to bleeding, look for:
- toothpaste for sensitive gums
- gentle, non-abrasive formulas that won’t irritate tissues
Should you visit the dentist regularly?
Absolutely, don’t wait for pain to show up. Make dental check-ups a regular habit – ideally every six months – or as often as your dentist recommends.
Always inform your dentist about your APS and any medications you’re taking. With this information, they can plan safe treatments, monitor your oral health more closely, and help you choose the best at-home products for your needs.
Antiphospholipid Antibody Syndrome isn’t just a blood condition; it can affect your entire body, including your mouth. From bleeding risks to mouth sores and gum disease, the effects go beyond what we usually think of as “just dental problems.”
The good news is that with proper hygiene, good communication with your healthcare providers, and regular dental care, most of these issues can be prevented or managed effectively.
Just remember: what happens in your body is also reflected in your mouth. Taking care of your oral health is part of taking care of your whole self.
Frequently Asked Questions
Can I get dental implants if I have APS?
Can APS make healing after dental work slower?
Is it safe to get a dental cleaning with APS?
Can APS increase the risk of oral infections?
Is it normal to have a metallic taste in the mouth with APS?
Voice and Search (Q&A)
Why is dental care important if I have APS?
People with APS often take blood thinners, which can cause bleeding during dental work. Good oral care helps prevent gum disease and reduce risks.
Can I get a tooth pulled if I have APS?
Yes, but your dentist must plan carefully with your doctor. They may adjust your medication and take extra steps to control bleeding during and after the procedure.
How can I protect my gums if I take blood thinners?
Brush gently with a soft toothbrush, floss with care, and visit your dentist regularly. Use fluoride toothpaste and alcohol-free mouthwash to avoid irritation.
Share
References
1. Cleveland Clinic. (2024, October 21). Antiphospholipid syndrome. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/21685-antiphospholipid-syndrome
2. D′Souza, D., Dandakeri, S., Bhat, M., & Srinath, M. (2015). An atypical presentation of antiphospholipid antibody syndrome. Indian Dermatology Online Journal, 6(4), 263. https://journals.lww.com/idoj/fulltext/2015/06040/an_atypical_presentation_of_antiphospholipid.6.aspx
3. Mayo Clinic. (2022, February 25). Antiphospholipid syndrome – Symptoms & causes. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/antiphospholipid-syndrome/symptoms-causes/syc-20355831
4. NHS. (2022, June 20). Antiphospholipid syndrome (APS). nhs.uk. https://www.nhs.uk/conditions/antiphospholipid-syndrome/
5. Okuyama, K., Naruse, T., Yutori, H., Yanamoto, S., Umeda, M. (2019). Oral surgery in patients with antiphospholipid syndrome. Journal of Oral Science, Vol. 61, No. 3, 386-390. https://www.jstage.jst.go.jp/article/josnusd/61/3/61_18-0164/_pdf
-
Dr. Yeidy Carolina Mesa [Author]
DDS Yeidy Carolina Mesa Passionate Dentist | Advocate for Accessible Oral Health Education Graduating from Universidad CES in 2022, I am a dedicated general dentist with a lifelong passion for helping others and making a meaningful impact in the world. My journey into dentistry began at the age of 7, inspired by my own experience with braces and overcoming a fear of the dentist. This personal journey shaped my mission to help patients conquer their own dental anxieties and embrace a healthier,...
View all posts
-
Nayibe Cubillos M. [Medical Reviewer]
Pharmaceutical Chemestry |Pharmaceutical Process Management | Pharmaceutical Care | Pharmaceutical Services Audit | Pharmaceutical Services Process Consulting | Content Project Manager | SEO Knowledge | Content Writer | Leadership | Scrum Master
View all posts
A healthcare writer with a solid background in pharmaceutical chemistry and a thorough understanding of Colombian regulatory processes and comprehensive sector management, she has significant experience coordinating and leading multidisciplina...