Last Updated on: 27th December 2025, 07:04 am
Sexually transmitted diseases (STDs) are often discussed in terms of overall reproductive and physical health, but their impact on oral health is usually overlooked. STDs are far more common than many people realize, with millions of new infections reported each year in the United States alone.
Believe it or not, your smile can also be affected, not just by visible oral symptoms or the possibility of infection, but by the medications, treatment side effects, and emotional toll that accompany STD care. These can gradually disrupt your oral care routine, sometimes without you even noticing.
From inflamed gums to persistent mouth sores or that annoying dry feeling in your mouth, things that seem unrelated to your treatment can start to show up every time you brush your teeth or try to eat.
We’ve created this clear and practical guide to help you understand what’s happening, the signs to watch for, and what you can do to take care of your oral health while managing an STD.
How STD care affects oral health

Not every STD manifests symptoms in the mouth, but the treatment itself, as well as its effects on your immune system, definitely have consequences for oral health. Let’s take a look at a few common reasons your mouth might start feeling different during this time.
Medications that cause dry mouth
Many treatments for STDs, like those for HIV, herpes, or HPV, often include antiretrovirals or antibiotics, which can reduce saliva flow.
This leads to dry mouth (xerostomia), and while it might seem harmless, it’s actually a big deal. Saliva protects your teeth from decay, helps control bacteria, and keeps your mouth feeling fresh. Without it, you’re more likely to experience cavities, bad breath, gum disease, and even difficulty eating or speaking.
Weakened immune system and oral infections
Some STDs, like HIV, weaken your immune system over time. A compromised immune system may leave you susceptible to bacterial infections or slower healing in the mouth.
This leaves the door open for problems like gingivitis, oral thrush (a fungal infection), persistent ulcers, and other complications that can interfere with daily comfort and your ability to eat or maintain hygiene.
Lifestyle and hygiene changes

Let’s not forget the emotional side. Living with an STD or going through treatment can feel overwhelming. You may be stressed, fatigued, anxious, or simply drained, and when that happens, oral hygiene easily falls by the wayside.
Skipping brushing or flossing now and then might not seem like a big deal, but over time, it can lead to bigger issues like gum disease, decay, or infections.
As you can see, several factors affect your oral health during STD care. Up next, we’ll go over the most common oral symptoms that may appear during this stage, so you can recognize them early and take proper care.
Common oral problems linked to STDs
STD treatment affects your oral health in different ways, through infection or treatment side effects. Let’s look at the most frequent symptoms and conditions to watch out for during treatment.
Mouth sores and ulcers
Certain STDs, like herpes simplex or syphilis, can cause painful sores or ulcers on your tongue, lips, gums, or the inside of the cheeks. These sores might look like common canker sores, but they often last longer, hurt more, or come back repeatedly.
If a sore doesn’t heal within a week or becomes a recurring issue, don’t ignore it; see a healthcare provider for proper evaluation and treatment.
Recommended products:
- Soothing oral gels for ulcers (look for hyaluronic acid or lidocaine)
- Antiseptic mouthwashes (e.g., chlorhexidine – always under medical supervision)
- soft-bristled toothbrushes to avoid aggravating lesions
Gum inflammation and bleeding (gingivitis or periodontitis)

When the immune system is weakened, as in cases of HIV, the gums become more vulnerable to inflammation, bleeding, and infection, even with gentle brushing. These are early signs of gingivitis, which, if not treated, can progress to periodontitis. This more severe condition damages the tissues that support the teeth and can eventually lead to tooth loss or painful infections.
Recommended products:
- Fluoride toothpaste for gum care
- Alcohol-free antimicrobial mouthwash
- Dental floss or water flossers for gentle cleaning
Dry mouth (xerostomia)
Many medications used in STD care, such as antiretrovirals or antibiotics, can reduce saliva flow. Dry mouth is more than a minor inconvenience. Without enough saliva, your mouth becomes a breeding ground for bacteria and plaque, leading to tooth decay, bad breath, and oral discomfort.
Recommended products:
- Sugar-free gum or lozenges with xylitol
- Saliva-stimulating sprays
- Alcohol-free moisturizing mouth rinses
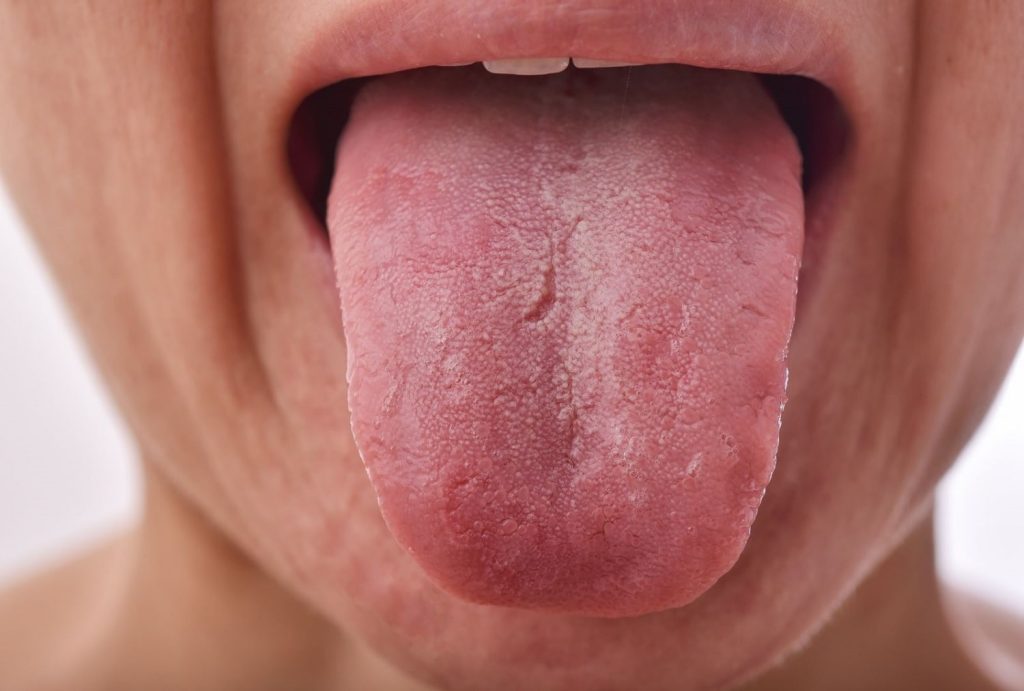
Oral thrush (candidiasis)
Oral thrush is a fungal infection caused by an overgrowth of yeast, often triggered by antibiotics, immune suppression, or a disrupted oral microbiome. It’s more common in people with weakened immune systems or those taking antibiotics; in individuals with HIV, it can be an AIDS-defining condition.
It typically shows up as white patches on the tongue, inside the cheeks, or on the roof of the mouth. These spots may cause burning, soreness, or a cottony feeling in the mouth.
Recommended products:
- Oral probiotics to restore healthy bacteria
- Antifungal mouth rinses or tablets (prescribed)
- Soft-bristle toothbrushes to reduce irritation
Supporting your oral health while managing STD care

Even if you’re going through long-term treatment, you can absolutely stay on top of your oral health with a few smart habits and a little consistency.
Here are some tips that can make a big difference:
- Prioritize regular dental visits: You might feel hesitant to bring up your health history, but your dentist is part of your care team. They can often detect signs of systemic issues, including STDs, through changes in your oral health, sometimes even before you notice them yourself. They will help you manage them safely and effectively.
- Stay consistent with hygiene routines: When you’re not feeling your best, brushing and flossing may not be your priority. But those few minutes a day can save you from major discomfort later on. Brush at least twice a day with fluoride toothpaste, floss daily or use a water flosser, and follow your dentist’s guidance on mouthwash choice. These habits protect against opportunistic infections and enamel erosion, especially when your immune system is weakened.
- Address mouth sores promptly: If you notice recurring ulcers or mouth wounds, don’t wait it out. Over-the-counter gels can help ease the discomfort, but the underlying cause needs medical attention, especially if your immune system is low.
Must-have products for oral health support

Caring for your mouth doesn’t have to be complicated. The right tools can help you stay comfortable and prevent serious issues. Here’s a basic list to keep on hand:
- Fluoride toothpaste with anti-inflammatory ingredients: strengthens enamel and soothes gums
- Alcohol-free antiseptic mouthwash: fights bacteria without causing dryness
- Xylitol-based gum or mints: stimulates saliva and helps fight bad breath
- Oral probiotics: support bacterial balance and may help reduce the frequency of oral thrush
- Soft-bristled toothbrush: Minimize irritation when brushing around sensitive gums or sores.
Avoid strong flavors, harsh whitening products, or alcohol-based rinses if your mouth is sensitive. And always consult your dentist before trying new products, especially if you’re undergoing medical treatment.
Conclusion
Managing an STD isn’t just about medications or doctor visits. It’s about taking care of your whole self, and that includes your mouth.
Even if oral health doesn’t seem like a priority at first, the truth is that it’s all connected. With a little awareness, the right products, and regular dental care, you can protect your smile and feel better in your everyday life.
Be honest with your dental care providers, follow your hygiene routine as best you can, and remember: caring for your oral health is part of caring for your sexual health.
Frequently Asked Questions
Why do my gums bleed more since I started STD treatment?
Is it okay to tell my dentist I’m being treated for an STD?
Is it safe to kiss someone if I have mouth sores?
How often should I replace my toothbrush during treatment?
Can I get an STD from oral sex, and will it affect my mouth?
Share
References
1. Loh, M. (2023). Sexually transmissible oral diseases. BDJ, 234(6), 372. https://doi.org/10.1038/s41415-023-5717-9
2. MouthHealthy. (s. f). Sexually transmitted diseases and your mouth. MouthHealthy – Oral Health Information From the ADA. https://www.mouthhealthy.org/all-topics-a-z/sexually-transmitted-diseases
3. NIH. (2018). HIV/AIDS & Oral Health. National Institute of Dental and Craniofacial Research. https://www.nidcr.nih.gov/health-info/hiv-aids
4. Oral sex and oral health – what you need to know. (2025, 14 January). Oral Health Foundation. https://www.dentalhealth.org/blog/oral-sex-and-oral-health
5. Scassia, A., Ferguson, S. (2023, 05 May). Oral STDs: What Are the Symptoms?. https://www.healthline.com/health/healthy-sex/oral-stds
-
Dr. Yeidy Carolina Mesa [Author]
DDS Yeidy Carolina Mesa Passionate Dentist | Advocate for Accessible Oral Health Education Graduating from Universidad CES in 2022, I am a dedicated general dentist with a lifelong passion for helping others and making a meaningful impact in the world. My journey into dentistry began at the age of 7, inspired by my own experience with braces and overcoming a fear of the dentist. This personal journey shaped my mission to help patients conquer their own dental anxieties and embrace a healthier,...
View all posts
-
Nayibe Cubillos M. [Medical Reviewer]
Pharmaceutical Chemestry |Pharmaceutical Process Management | Pharmaceutical Care | Pharmaceutical Services Audit | Pharmaceutical Services Process Consulting | Content Project Manager | SEO Knowledge | Content Writer | Leadership | Scrum Master
View all posts
A healthcare writer with a solid background in pharmaceutical chemistry and a thorough understanding of Colombian regulatory processes and comprehensive sector management, she has significant experience coordinating and leading multidisciplina...Recent Posts